-
11 July 2025 | Country Update
Amendment of the Act on Health Services: Enhancing emergency care and patient rights, and reducing bureaucracy -
25 November 2023 | Country Update
The right to be forgotten
2.8. Person-centred care
2.8.1. Patient information
Since 2007, patients or designated persons have full access to their own medical records from providers and may make a copy (or ask the provider for a copy, which may be subject to a fee). Based on the Health Service Act (2011), providers must inform patients about their health status and alternative treatment options, including about the appropriateness, risks and benefits of all alternative treatments (see Table2.2).
Table2.2

HIFs allow their members (physically or electronically) to view the care that they were provided which was reimbursed to providers (see section 4.1.3). Additionally, patients can view their prescription pharmaceutical records via the electronic prescription system. As some prescription pharmaceuticals are not fully covered by SHI, patients have the right to be informed by their physicians and pharmacists on available pharmaceuticals with similar therapeutic effects and lower or no co-payments (generic substitution).
According to the Health Insurance Act (1997), HIFs must guarantee accessible care to their members within a reasonable time frame in their area of residence. Accessibility times differ by specialization and are set by the government (Governmental Regulation no. 307/2012 Coll.). Both the Czech Medical Chamber and the Czech Dental Chamber provide public lists of physicians and dentists that patients can consult to find care (https://www.lkcr.cz/seznam-lekaru-426.html, https://www.dent.cz/zubni-lekari/, respectively). All providers with valid registration are also included in the National Register of Healthcare Providers. If a patient cannot register in their area of residence (for example, because contacted physicians are not accepting new patients), they may contact their HIF to ask for assistance in finding an available provider; HIFs provide lists of providers in the area, though these also include providers not admitting new patients (so often these lists are not very helpful). Providers can only reject new patients for a few reasons.
- due to capacity, which is vaguely defined (each provider sets its own capacities), though overcapacity would mean a decrease of quality with every additional new patient;
- GPs can reject patients if the distance from their residence would hamper regular visits; or
- if a patient is a member of a HIF that a provider is not contracted with.
Patients generally do not have access to information from the internal quality assessments of providers, and there is no unified methodology implemented that would enable patients to make informed choices. Data from performance measurements for stakeholders, though for decision-making purposes and quality improvements, may also be published for the public, such as from the HIB (2021). A patient under 18 years of age has a say in health service provision. Their opinion must be considered as a factor, increasing in importance with age.
To boost health literacy in Czechia, MZČR launched the NZIP, developed by ÚZIS through EU funds, to provide verified information on various health topics, including specific diseases, allergens and vaccinations, and on prevention and healthy lifestyles, among others. The portal also includes information on existing patient organizations (https://www.nzip.cz/kategorie/45-pacientske-organizace). The accuracy of information featured on the NZIP is guaranteed by MZČR and is collected with the help of medical experts from ČLS JEP.
Attempts have been made to address the information needs of minority populations and HIFs publish general information about the Czech health system in Vietnamese and Ukrainian languages (larger minority groups). Individuals with health conditions enjoy the same membership benefits and pay the same contributions as all others. To reflect the needs of the visually impaired, manufacturers have been required to include Braille text on consumer pharmaceutical packaging since 2007. For the hearing impaired, patient rights have been explained using sign language on video recordings. Additionally, a council representing patients was re-established in 2017 as an advisory body to MZČR (see section 6.1); council members are asked to comment and give suggestions to changes in legislation, actions and measures, and thus serves as a mediator between patients and their needs and MZČR.
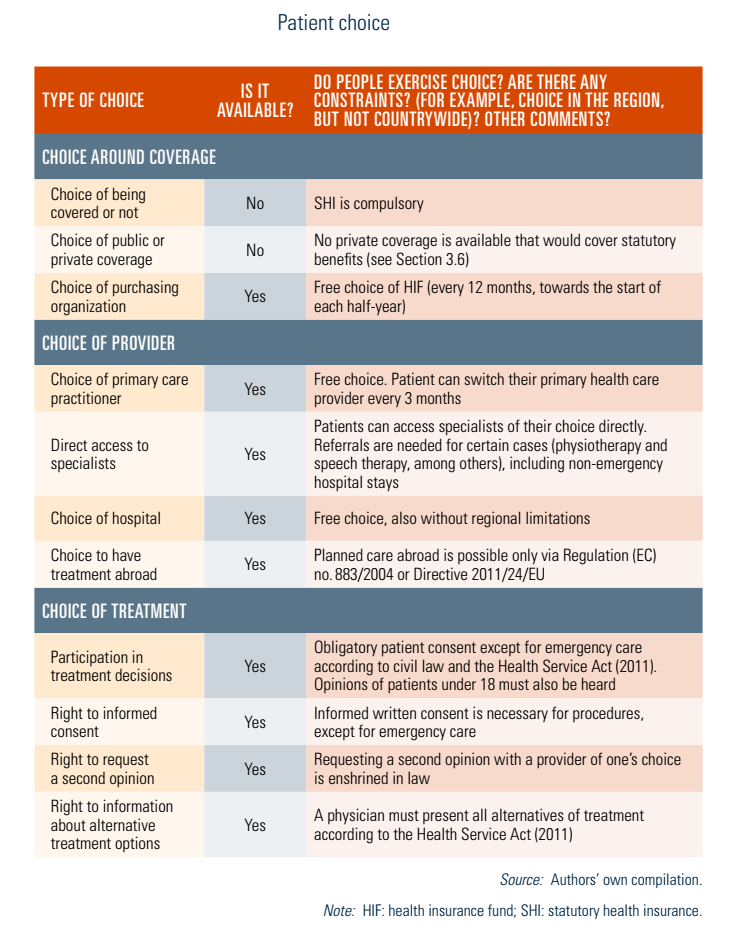
2.8.2. Patient choice
Generally, no one can opt out of health insurance in Czechia. Insured individuals, however, have the right to choose their HIF freely and have free choice of provider. In regard to HIFs, patients may switch their HIF once every 12 months, always towards the start of each half-year, that is either by 1 January, or by 1 July.
All HIFs are obliged to accept any applicant; risk selection is not permitted. There is hardly any competition among HIFs. They cannot deviate from the basic benefits package, but they can offer supplementary programmes to which they provide small contributions (for example, self-paid swimming courses by members, voluntary vaccinations). These fees are very small, being around CZK 925 per activity course in 2020.
Patients also have the right to choose or switch their primary health care provider every three months (see Table2.3). According to the Health Service Act (2011), a provider must inform patients about all alternatives and suggested forms of treatment, though instances of this not occurring are still being reported. In practice, providers often only present their preferred alternative(s).
Table2.3
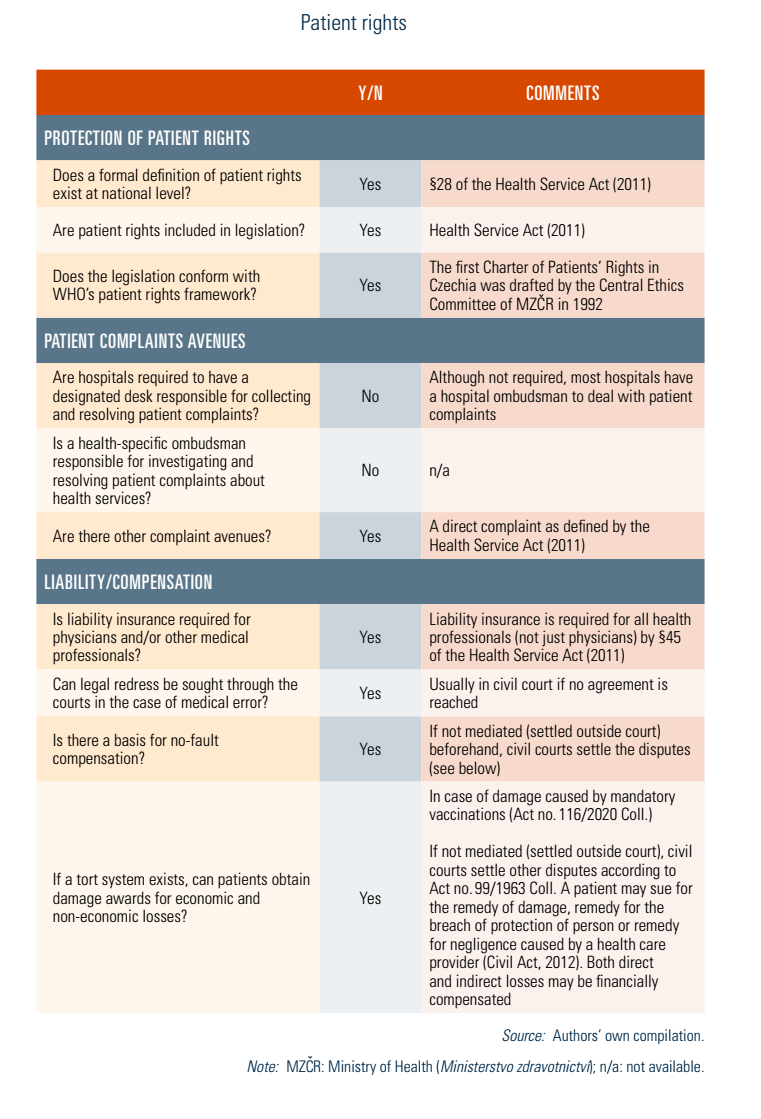
2.8.3. Patient rights
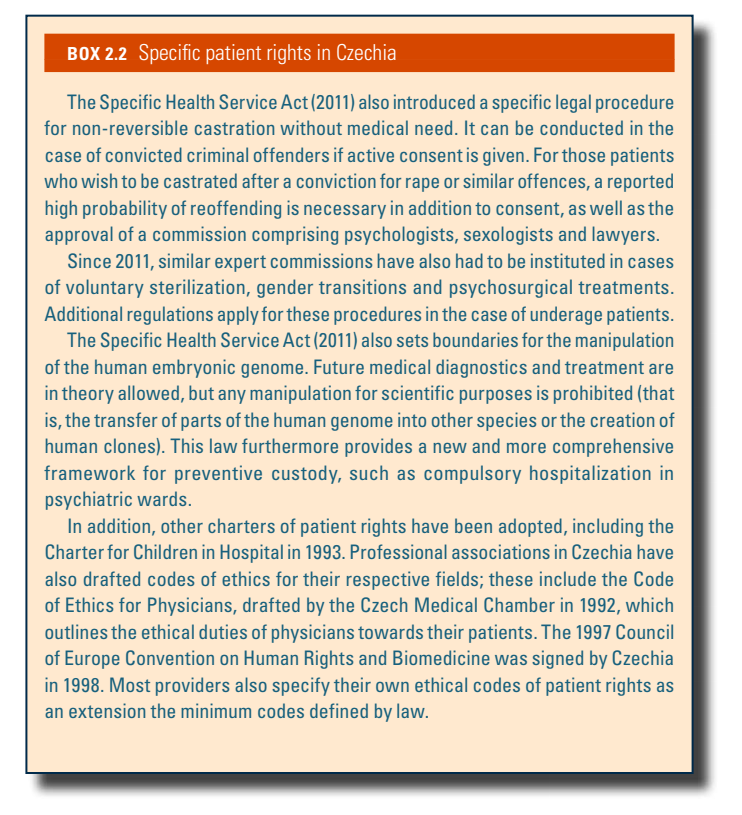
Patient rights were substantially re-specified in the Health Service Act (2011). Patients have the right to choose their physician and hospital freely; to have guaranteed access to care within reasonable time limits in their area of residence (as defined by Governmental Regulation no. 307/2012 Coll.); to seek a second opinion; to receive medical treatment according to recognized standards; to determine the treatment and its extent; to have medical procedures performed only with their legal consent; to view their own medical records and copy them; to have their patient data treated with confidentiality; to access a translator at all times in case of inability to communicate; to living wills (expressly excluding assisted suicide); and to receive compensation in the event of medical error, lack of informed consent, or injury caused by pharmaceuticals or medical devices. The Health Service Act (2011) further regulates rights of the children, and the Specific Health Service Act (2011) includes provisions on sterilization, in vitro fertilization (IVF), organ donation and specific patient rights related to these services (see Box2.2).
Box2.2
Complaint procedures are defined by the Health Service Act (2011), which stipulates who can file a complaint against a provider; the burden of proof lies with the filer. Providers must respond within 30 days to the complaints filed, and persons unsatisfied with the providers’ handling of the complaint can subsequently inform the respective administrative body (primarily regional governments). There are also precise rules for setting up exploratory committees and/or consulting professionals, if necessary, to decide the legitimacy of a complaint. In case of compensation requests, the matter is usually settled by civil courts. Even though the Health Service Act does not stipulate it explicitly, patients may also contact their HIF if the provider rejects carrying out a procedure covered by SHI. Professional chambers may be contacted particularly if ethical codes have been breached. More specifically, Act no. 116/2020 Coll. defines rights and complaint procedures in cases of damage caused by compulsory vaccinations. Table2.4 elaborates on the extent of patient rights in Czechia.
Table2.4
A major change is the transfer of responsibility for organizing emergency services (pohotovostní služby) from regions to health insurance funds, which is expected to improve equitable access by leveraging insurers’ greater capacity.
The reform also bolsters patient rights and protection by:
- introducing hospital ombudsmen to handle complaints directly within facilities,
- strengthening protections for patients at risk of domestic or sexual violence, and
- strengthening the right to transparent information about the cost of healthcare services and significantly tightening penalties for illegal fees charged by doctors.
The amendment also establishes centres for comprehensive care for children with long-term health conditions. These centres will provide coordinated, multidisciplinary care to improve the quality of life for paediatric patients and help families navigate the healthcare system more easily.
In November 2023, the Czech Insurance Association (ČAP) issued a recommendation for its members on life insurance for individuals who have recovered from an oncological disease (cured cancer patients). On this recommendation, insurance companies pledge to create a list of oncological diagnoses and time periods. When these time periods elapse, an individual’s oncological history will be “forgotten” when applying for life insurance and financial services, and they will be treated the same as someone without a history of oncological treatment(s) and under standard conditions. Each involved insurer will make the list of diagnoses and periods publicly available. The periods are expected to be around seven years, depending on the individual’s age and type of cancer. The recommendation is binding for those insurance companies that accede to it.
ČAP, which supports the interests of insurance and reinsurance companies, acknowledged the positive development in the research and treatment of oncological diseases. It reflects data from the Institute of Health Information and Statistics of the Czech Republic and discussions with patient organizations at the Ministry of Health.
Authors
References
Czech Insurance Association (2023). ČAP self-regulatory standard for approach to persons who have experienced cancer in the context of life insurance. [Samoregulační standard ČAP pro přístup k osobám, které prodělaly onkologické onemocnění, v kontextu životního pojištění]. Available at: https://www.cap.cz/odborna-verejnost/samoregulacni-standardy.
Ministry of Health (2023). Cured cancer patients will have equal access to financial services. Representatives of the Ministry of Health, patient organisations and the financial sector agreed on the “right to be forgotten”. [Vyléčení onkologičtí pacienti budou mít rovný přístup k finančním službám. Na “právu být zapomenut” se shodli zástupci Ministerstva zdravotnictví, pacientských organizací i finančního sektoru]. Press release issued on 9 October 2023, updated on 17 October 2023. Available at: https://www.mzcr.cz/tiskove-centrum-mz/vyleceni-onkologicti-pacienti-budou-mit-rovny-pristup-k-financnim-sluzbam-na-pravu-byt-zapomenut-se-shodli-zastupci-ministerstva-zdravotnictvi-pacientskych-organizaci-i-financniho.
Zdravotnický deník (2023). Cured cancer patients will be considered healthy by insurance companies. [Vyléčené onkologické pacienty budou pojišťovny posuzovat jako zdravé]. Issued on 9 October 2023. Available at: https://www.zdravotnickydenik.cz/2023/10/vylecene-onkologicke-pacienty-budou-pojistovny-posuzovat-jako-zdrave.
2.8.4. Patients and cross-border health care
There are several ways to receive care abroad. As EU citizens, Czechs can use their European Health Insurance Card to receive services abroad. This is paid for by the Czech system when temporary stays result in cases of emergency care (as tourists, for example). For planned care abroad, Regulation (EC) no. 883/2004, supplemented by Regulation (EC) no. 987/2009, may be used. It requires prior consent of a Czech HIF and covers full costs for patients in the approved foreign country or countries. Planned care can also be sought under Directive 2011/24/EU, where no prior authorization (as opposed to other EU countries) is required. In this case, patients cover all costs of care in another member state and subsequently file reimbursement claims up to the costs usual in Czechia with their HIF. Patients are responsible for any price differences.
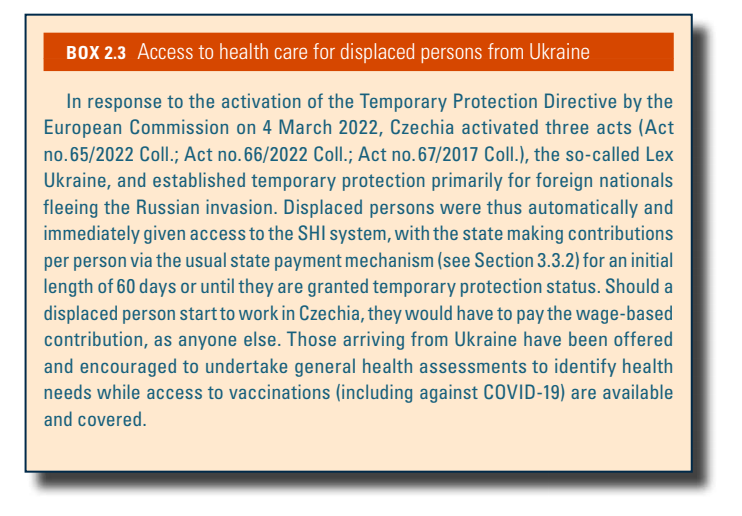
Cross-border reimbursements for Czech patients abroad and claims for costs paid for foreign nationals in Czechia are settled through the HIB. Cross-border health care is not widely applied in Czechia, though. According to HIB statistics, planned care provided to Czech patients abroad in 2020 (according to the directive regimen) totalled 106 cases (accounting for 2% of costs of care provided to Czech patients abroad), whereas as many as 1329 insured Europeans received planned health care in Czechia, including 1020 Slovaks, 144 British individuals, 58 Croatians and 39 Germans. In 2020, Czechia issued a total of 116 S2 certificates for cross-border cases (according to the regulation regimen), including 47 cases for Germany, 31 for Slovakia, 13 for Poland and 8 for Austria (HIB, 2020). Care has been made accessible for displaced persons from Ukraine (see Box2.3).
Box2.3