-
26 September 2025 | Country Update
A new RSV vaccination programme was launched in autumn 2025 to prevent severe illness and hospitalizations in infants -
25 March 2025 | Country Update
New agreement on the use of electronic age verification solutions in retail stores -
23 May 2024 | Country Update
New political agreement on legislative changes to abortion -
19 December 2023 | Policy Analysis
Political agreement on a new prevention plan aims to reduce children and youth’s consumption of alcohol, nicotine products, and tobacco
5.1. Public health
Respiratory syncytial virus (RSV) infections lead to hundreds of infant hospitalizations each year in Denmark, particularly among those under three months old.
To prevent disease and hospitalizations among infants, the government has launched a new RSV seasonal vaccination programme for pregnant women; they will be offered the vaccine during a pregnancy check-up with their doctor in the 32nd week of pregnancy.
Initially planned for May 2026, the programme was launched earlier, with pregnant women offered the vaccine starting in autumn 2025 to provide earlier protection during the peak RSV season. The government proposes to allocate DKK 35.9 million (€4.8 million) in 2026 and DKK 40.2 million (€5.4 million) in 2027 to introduce the new vaccination programme.
Authors
References
Nyt vaccinationsprogram skal forebygge alvorlig sygdom hos spædbørn | Indenrigs- og Sundhedsministeriet
As of March 2025, the legal age for buying alcohol with a percentage between 1.2% and 16.5% is 16 years, and the age limit for purchasing alcohol with a percentage higher than 16.5%, e-cigarettes, nicotine products and tobacco is 18 years. Despite these regulations, retail stores often illegally sell these products to minors [1].
The government and the parties behind the prevention plan [2] have agreed to allow retailers to use electronic age verification solutions to prevent the sale of alcohol, tobacco and nicotine products to minors. If a solution meets minimum requirements, retailers can choose which ones to accept. Implementing electronic age verification requires a legal amendment, with a bill expected in the 2025/2026 parliamentary session [1].
The agreement is part of a broader prevention plan with 30 initiatives aimed at delaying children and adolescents’ first exposure to alcohol and restricting access to tobacco and nicotine products [2].
Authors
The government has reached a broad political agreement to extend the free abortion limit from the end of the 12th gestation week to the end of the 18th gestation week. Moreover, this agreement includes replacing the five regional abortion committees with a national abortion board and providing 15- to 17-year-olds with the opportunity to obtain an abortion without parental consent. If a woman wishes to terminate the pregnancy after the 18th gestation week, she must apply to the national abortion board.
The rationale behind the new agreement is to give women more time and opportunity to act on the information they receive from foetal medical examinations, thereby enhancing their autonomy. The new legislation is expected to take effect on 1 June 2025.
Authors
In November 2023, a prevention plan with 30 specific initiatives to prevent and reduce the consumption of nicotine products, tobacco, and alcohol among children and youth was reached as a political agreement between the government and four opposition parties.
The background for the new prevention plan stems from the emergence of new smoke-free nicotine products in recent years, particularly among children and youth who have shown an increased interest in these products. The nicotine products are not only harmful to health but also highly addictive, serving as a stepping stone for children and youth to start smoking. Additionally, Danish children and youth also exhibit high alcohol consumption compared to their peers in other European countries. Furthermore, they initiate alcohol consumption at an earlier age. Despite being illegal, minors can easily access age-restricted products that are widely sold to them.
To curb this trend and halt illegal sales, an allocation of nearly DKK 500 million (€67 million) has been designated for implementing the 30 initiatives in the prevention plan.
Key points of the agreement include:
- The agreement prohibits 16-to-17-year-olds from purchasing alcohol with an alcohol percentage exceeding six per cent. Currently, it is legal to sell products with an alcohol percentage of up to 16.5 to this age group. While the sale of regular beer to this age group remains legal, stronger alcoholic products, such as wine and shots, are now prohibited.
- The tax on smoke-free nicotine products is raised from 5.5 to 10 øre (penny) per milligram of nicotine. This results in an average price increase of around DKK 12 (€1.6) for a can of nicotine pouches, aligning the cost more closely with a pack of cigarettes.
- Similar tax increases are implemented on smoke-free tobacco, including chewing tobacco, to prevent unintended substitution between different products.
- The penalty levels for violating rules related to tobacco and nicotine products are raised, with fines starting at DKK 50,000. This applies to both the illegal marketing of tobacco and nicotine products in Denmark and the illegal sale of tobacco, nicotine, and alcohol to minors.
- The agreement imposes requirements on the placement of alcoholic beverages in retail and a ban on “enticing” flavours and scents in tobacco substitutes.
Authors
5.1.1. Organizational set-up and main institutions
The responsibility for public health services is dispersed between different actors. Public health services are partly organized as separate activities run by the municipalities and specific institutions and partially integrated with curative services under the regions (see section 2.1).
The municipalities must: promote health and prevent diseases for all citizens, which includes special activities such as health visiting nurses for infants, school nurses and preventive home visits for older people; offer general and free health prevention information; organize health preparedness in emergencies (e.g. war, terrorism, dangerous infectious disease outbreak); report information to central health authorities and cooperate with the regions, including general practice. Municipality health promoting and preventive efforts are guided by the prevention packages on selected public health issues, for example, alcohol, physical activity and hygiene, issued by the Danish Health Authority. These knowledge-based tools with professional recommendations can contribute to prioritizing and developing high-quality municipal prevention work. Individual municipal councils prioritize their efforts and set the level of services, but they must meet the requirements and frameworks in the Health Act. Municipal tasks aim to emphasize public health interventions versus curative care with a decentralized approach.
According to the Health Act, the regions also have a responsibility for prevention and an advisory role for the municipalities which is partly based on their responsibility for completing the National Health Profile. In recent years, the regions have focused more on preventive efforts; for example, by launching funds for prevention research and initiating an appeal for a public health law. From July 2022, new health clusters have been established and one task of the clusters is to coordinate disease prevention and health promotion activities (see section 5.2).
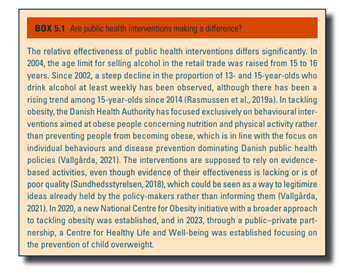
Under the auspices of the Ministry of Health, the Danish Health Authority carries out different public health functions, including advice on health promotion, disease prevention and the child vaccination programme. It also assesses the national screening programme and contributes to managing emergencies, outbreaks and other infectious diseases. The Danish Health Authority’s advisory role covers noncommunicable diseases, sexual health, tobacco control, physical activity, mental health and alcohol- and drug-use directly to the public, the central government, the regions (including health professionals) and municipalities. Health promotion and prevention advice is communicated mainly via booklets, websites and campaigns and through reports on active management programmes for noncommunicable diseases. The three prevention packages on tobacco, alcohol and mental health have been prioritized by the municipalities (Jakobsen, Sølvhøj & Holmberg, 2020). Protective factors and structural efforts receive less attention in the prevention packages (Box5.1).
Box5.1
The Danish Health Authority also assesses the content of existing national screening programmes and adjusts them regularly via professional recommendations and advice. Furthermore, the Danish Health Authority coordinates several population surveys in close collaboration with the National Institute of Public Health and the regions to monitor the health and health behaviour of the population. The Danish Health Authority also contributes to managing infectious disease outbreaks, such as preparing national strategies and guidelines for the authorities. Similarly, the Danish Health Authority is part of the national emergency preparedness in Denmark. It cooperates with other authorities on emergency planning and has a permanent place in the national staff that meets if there is an emergency incident.
The primary responsibility for surveillance and control of communicable diseases rests with the National Serum Institute (Statens Serum Institut), which also assists in identifying sources of infection in foodborne disease outbreaks. GPs and hospital doctors are obliged to report cases of certain communicable diseases to the Danish Patient Safety Authority (under the Ministry of Health), which oversees individual and community interventions to prevent the spread of communicable disease(s). Furthermore, the Danish Patient Safety Authority advises on communicable diseases, water pollution and chemical spills as part of the societal preparedness plan. While their function is mainly advisory, they have the power to implement measures to prevent the spread of infection. This work is carried out in collaboration with the National Serum Institute and the Danish Health Authority.
Under the Ministry of Employment, the Danish Working Environment Authority monitors and maintains occupational health and safety standards. Inspecting workplaces, regulation and information aims to promote safe and healthy work environments. The provision of these tasks, together with their power to issue administrative fines or to order work to be suspended if the workplace does not comply with health and safety rules, makes the Danish Working Environment Authority an influential actor in the public health arena.
5.1.2. National public health programmes
Since 2009, no new national public health programmes have been issued despite Denmark’s slow increase in average life expectancy since 2000 and the observed growth in health inequalities (Sundhedsstyrelsen, 2020a; 2022b; Møller, 2023). There is a much larger focus on curative care than on health promotion and disease prevention, which is also reflected in the 2022 health reform and the allocation of funds and research grants. However, political strategy papers have an underlying perception that more preventive efforts are needed to reduce the increasing pressure on the health care system.
Previous national public health programmes have focused more on health-related behaviour and less on social and structural factors that influence health (Vallgårda, 2010; 2011; 2021). One exception is tobacco control: smoking is not allowed indoors in workplaces, restaurants and large pubs (2007); young people under the age of 18 years are banned from buying tobacco (2008); the price of a pack of cigarettes has risen from DKK 40 (€5.4) to DKK 55 (€7.4) (2020) and to 60 DKK (€8) in 2022; and smoking at schools and leisure facilities is prohibited (2021). The latter law is part of the former Social Democratic government’s national action plan against children and young people smoking with the ambition that no children and young people should smoke by 2030 (Sundheds- og Ældreministeriet, 2019b).
At the regional and local level, in 2017, the Danish Regions published Health for life – prevention is a necessary investment that included four strategy tracks as a dialogue invitation to other health actors to create more healthy life years by increased preventive efforts (Danske Regioner, 2017). In 2018, Local Government Denmark launched the Prevention in the Future strategy with six landmarks to set a common direction for the municipalities’ work to strengthen preventive efforts (Kommunernes Landsforening, 2017). In 2020, the Danish Regions pushed, together with several public and private institutions, for a public health law (Danske Regioner, 2020), but, at the time of writing, Local Government Denmark has not signed the appeal.
5.1.3. National screening programmes
Currently, three national systematic disease-specific screening programmes are in place: cervical cancer, breast cancer and colorectal cancer. From 2024 as part of cancer plan V, the coalition government will launch a three-year pilot study of screening for lung cancer, to uncover the organizational, resource and technological possibilities for a national screening programme for lung cancer. The regions are responsible for operating and monitoring all screening programmes. The national screening programme for cervical cancer has been running since 1986 and is offered to all women aged 23–64 years: every third year for women aged 23–29 years and every fifth year for 60–64-year-olds. For women aged 30–59 years, a randomized controlled trial has been set up randomizing women born on an even or uneven date, respectively, to being offered screening either every third year or every fifth year. Systematic breast cancer screening (mammography) has been in effect since 2007 and is offered to women aged 50–69 years every other year. Since 2014, screening for colorectal cancer has been offered to all citizens aged between 50 and 74 years every other year.
All pregnant women are offered screening for hepatitis B, HIV and syphilis at the first pregnancy examination by their GP. The examination is optional and is part of the routine blood samples taken during pregnancy, and the participation rate is high (nearly 100% in 2019) (SSI, 2020). In addition, all pregnant women have access to antenatal services provided by GPs, midwives and with medical indication to obstetricians in hospital obstetric departments. All neonates are offered screening for several congenital diseases, including metabolic disorders, via a heel-prick blood test, and screening for hearing impairment.
5.1.4. National plan on infectious diseases
The Act on Measures against Infectious and Other Communicable Diseases (1980, last updated 2021) lays down the legal framework for the Danish authorities’ prevention of serious infectious diseases. The diseases covered by the Act are divided into two lists: List A concerns diseases defined as “generally dangerous” (diseases with a high risk of infection, a usually serious course, and often high mortality), such as smallpox, Ebola and plague; List B relates to other infectious diseases, such as cholera, typhus, influenza, etc. The Act does not cover sexually transmitted infections. Doctors are obliged to report certain diseases to the Danish Patient Safety Authority and the National Serum Institute. The Danish Patient Safety Authority has day-to-day responsibility for preventing the spread of infection. The National Serum Institute monitors the incidence of disease (Sundheds- og Ældreministeriet, 2020a; 2020b).
In 2021, a new Act was adopted, which made it possible to impose measures on individuals, including assembly bans and the obligation to provide personal data to the Minister of Health if deemed necessary to prevent the spread of a dangerous infection, but not compulsory vaccination (Sundheds- og Ældreministeriet, 2021a). The new Act strengthens governmental control over the handling of epidemics. It gives far-reaching powers to the Minister of Health while at the same time has disputed elements of coercion, which challenge citizens’ legal security. Yet, the Act has also laid down a new parliamentary committee to control the Minister’s decisions, the establishment of a new national epidemic commission to advise the Minister of Health and other ministers on the management of socially critical diseases, as well as an automatic judicial review in cases of deprivation of liberty. Some experts claim that the Act is based too much on the experiences of the COVID-19 pandemic and lacks general preparedness for future scenarios.