-
26 September 2025 | Country Update
Reform of general practice: Balancing patient load and professional input -
23 May 2024 | Country Update
New political agreement on legislative changes to abortion -
23 May 2024 | Country Update
New agreement on partner egg donation without health-related justification
5.3. Primary care
GPs play a key role as the first point of contact for patients. They have numerous and varied tasks. They investigate, diagnose and treat suspected diseases; filter and refer patients to the specialized health care system; perform routine checks for well defined chronic conditions and preventive examinations of pregnant women and children and special groups; and certify health conditions and diseases for third parties. Finally, they have a coordinating role in the health care system, focusing on cooperation within the municipalities and sector transitions. Their work assignments are laid down in an agreement between Danish Regions and the Danish Organization of General Practitioners.
Patients can freely choose their GP from the practices with availability and change their GP for a small fee. There is a slight variation in the number of inhabitants per GP across regions. For example, in 2022, there were 60 GPs per 100 000 inhabitants on a national basis (ranging from 56 in the Region Nordjylland to 65 in the Region Syddanmark). This means that all patients have a relatively short distance to their GP, and geographical access to GP services is relatively equitable (Box5.2). However, some regions have experienced significant difficulties with recruitment, particularly in rural and socially disadvantaged urban areas. In 2018, it was estimated that around 1.8 million citizens lived in areas with low GP coverage (PLO, 2019a). To mitigate shortages of GPs in some areas, in 2017, a broad political agreement allowed the regions to operate medical clinics and allowed GPs to establish branch facilities staffed with employed physicians. In 2022, the health reform further extended the specialist medical education part in general medicine with correspondingly less time based in hospitals and gave the regions the opportunity to provide a special financial subsidy for a limited period and in certain areas with a shortage of GPs. The number of GPs is expected to increase by 43% from 2022 to 2035. Utilization of GP services was stable from 2009 to 2019, with approximately 41 million contacts per year, albeit with increasing email consultations (Danmarks Statistik, 2020a). This is equivalent to seven GP contacts per capita annually.
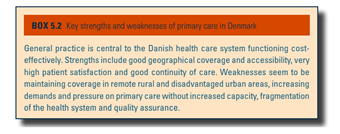
Box5.2
GPs run private practices, either as solo practitioners or in collaboration with other GPs in group practices. The general trend shows an increasing number of group practices, from 27% of general practices in 1977 to 59% in 2022 (PLO, 2022b). GPs derive their income from the regions according to a tariff negotiated by the Organization of General Practitioners and Danish Regions (see section 3.7.2). The GPs are responsible for practice costs, including buildings (rented or owned) and staff.
There are targeted quality development programmes for general practice. These include Data Capture, which ensures that each practice has the capacity for quality monitoring and development through performance data within type 2 diabetes and COPD care. The Quality in General Practice programme aims to promote and support all GPs in finding professional clusters which meet and work with quality data and quality development. No other quality indicator programmes exist within general practice. General practice clinics underwent one round of accreditation from 2016 to 2019. Practices not wanting to participate in this programme must submit to an accreditation-like control procedure. A nationwide survey of over 121 000 patients in 2018 showed patients generally having very high satisfaction with their GPs. Patients were most satisfied with the doctor–patient relationship (97% rate it as exceptional, very good or good). In comparison, accessibility received the lowest scores (88% rate it as exceptional, very good or good) (PLO, 2019b).
Denmark is currently embarking on a new health reform, and in the summer, the first bill was sent out for public consultation. The bill was generally well-received, but the Danish Medical Association (PLO) urged the Danish government to clarify and amend specific points in the bill. The Danish government and the PLO have agreed on a framework for a legislative package aimed at strengthening primary care and developing general practice.
For example, in the draft bill, general practitioners (GPs) with fewer sick patients will take on more patients, while those with the most complex caseloads will see fewer patients. The PLO was concerned about potential income effects for busy GPs, specifically whether they would earn the same amount while seeing more patients. To address this, an additional DKK 482 million (€64.5 million) will be allocated from 2027 to 2032 to compensate GPs, particularly in larger cities, who take on more patients.
A new professional council will also be established, with four of its eight members being GPs and the rest representing the regions, the Ministry, and the Danish Health Authority. The council will provide input on GP tasks, but final decisions on task descriptions will remain with the Danish Health Authority.
Authors
References
Regeringen og PLO er enige om kursen for udviklingen af almen praksis | Indenrigs- og Sundhedsministeriet
Fælles forståelse af reformen af de almenmedicinske tilbud.pdf
The government has reached a broad political agreement to extend the free abortion limit from the end of the 12th gestation week to the end of the 18th gestation week. Moreover, this agreement includes replacing the five regional abortion committees with a national abortion board and providing 15- to 17-year-olds with the opportunity to obtain an abortion without parental consent. If a woman wishes to terminate the pregnancy after the 18th gestation week, she must apply to the national abortion board.
The rationale behind the new agreement is to give women more time and opportunity to act on the information they receive from foetal medical examinations, thereby enhancing their autonomy. The new legislation is expected to take effect on 1 June 2025.