-
05 December 2025 | Country Update
New reform on patients sent abroad for cross-border care -
05 May 2025 | Country Update
A rise in patient complaints between 2022 and 2025
2.8. Person-centred care
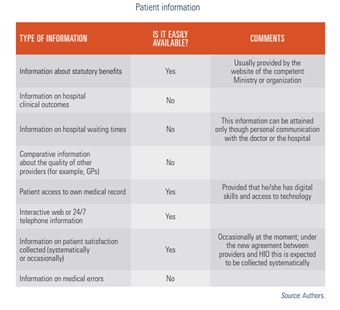
2.8.1. Patient information
The GeSY portal (https://www.gesy.org.cy/launchpad.htm) provides patients with access to information regarding enrolment processes, health care providers and services covered by the system, costs of treatments and co-payments, their rights and obligations, relevant legislation, annual reports, as well as access to their medical record and the medical record of their children until the age of 18. This information is provided in both Greek and English; however, the beneficiary must have the necessary digital skills to access it.
There is also a telephone line which provides immediate assistance and support to citizens. Information regarding the contracted HIO providers, as well as working hours and days can also be found on the website of both public and private hospitals. Information on waiting lists is only available through personal communication with the doctors or hospitals. No official information is available on hospital clinical outcomes or medical errors.
Challenges in accessing information can exist for third-country nationals. This is especially so for those who do not speak or read English as the language barrier makes it difficult for them to access all relevant health information and to communicate with providers (Kantaris, Theodorou & Kaitelidou, 2019; Panayiotopoulos, Apostolou & Zachariades, 2019). There is also no official information on hospital clinical outcomes, waiting lists and medical errors, as shown in Table2.2.
Table2.2
2.8.2. Patient choice
Within the GeSY, beneficiaries have more choice from a much larger number of providers, in both the public and the private sectors. In addition, they have the right to choose their personal doctor, who they can change after the completion of 12 months if desired (see Table2.3), stating the reason for the change. Beneficiaries can also choose a hospital or visit a specialist of their choice, following a referral from their personal doctor. Patient choice is facilitated by sufficient information on the HIO website, ensuring good knowledge of the system by beneficiaries.
Table2.3
2.8.3. Patient rights
The basic rights of patients within the GeSY – namely rights to health care and treatment, freedom of choice and equal access to all legal residents – have been achieved to a great extent. Nevertheless, there remains room for improvement in issues such as confidentiality, quality of services, safety, avoidance of suffering and pain, making a complaint and compensation.
According to the relevant legislation (The Safeguarding and Protection of Patients’ Rights Law of 2004), every public hospital is obliged to have a person responsible for patients’ rights. Among their responsibilities are sending complaints for further investigation to the Complaint Review Committees, which have been set up in all districts, to defend and promote patients’ rights. These committees are responsible for investigating complaints of first and second degree relating to the private sector as well as public hospitals, sent to them either by the Patients’ Rights Officer, or complaints from patients who are not satisfied with the Officer’s decision. In addition to the above, both the Supervisor Commissioner of the GeSY and the HIO have the authority to deal with complaints. See more details in Table2.4.
Table2.4
However, the OSAK argues that patients’ rights are not fully guaranteed in practice, and there have been several complaints from patients for violating the provisions of the relevant law. For this reason, the MoH is considering the possibility of creating a specific ombudsman for patients, to better inform them of their rights and to more effectively ensure their rights in practice. The introduction of the relevant bill to the Parliament for voting is still pending.
The Patients’ Rights Observatory, run by the Cyprus Federation of Patients’ Associations, plays a central role in monitoring healthcare and advocating for patients’ rights in Cyprus. Between 2022 and early 2025, the observatory recorded an increase in patient complaints – up 44.9% in 2023 compared to 2022. Although these complaints (see Table 1) are not a direct measure of satisfaction, they provide valuable insights into the ongoing challenges and changes in public expectations regarding the GeSY.
Table 1. Main categories and selected share of complaints. (Note: these shares only tally up to 90%.)
| Main categories | Share of total complaints | Key issues |
| Medications | 32% | Non-coverage by GeSY, variable copayments |
| Access to services | 19% | Delays in appointments, long waiting times in emergency departments or to see specialists |
| Behaviour of healthcare professionals | 17% | Poor conduct and communication |
| Expenses and costs | 14% | Unexpected charges at point of service (copayments and contributions) |
| Quality of services | 8% | Concerns about adequacy |
Source: authors’ own elaboration based on data from https://cypatient.org/observatory-information.
A recent and notable trend is the emergence of complaints from personal doctors within GeSY who report being pressured by patients to issue referrals, while at the same time facing strict monthly referral limits from the HIO. This tension has led to dissatisfaction on both sides: patients report being denied the specialist care they need, and providers express concerns that their clinical autonomy is being compromised.
2.8.4. Patients and cross-border health care
Directive 2011/24/EU of the European Parliament “on the application of patients’ rights in cross-border healthcare” and the respective national legislation, the “Law for the Application of Patients’ Rights in Cross Border Healthcare 2013”, provide patients with more cross-border rights and choices, in line with the objectives of the EU single market. Both clearly declare that patients have the right to seek treatment abroad and be reimbursed for the amount they would have been reimbursed if they had been receiving the same treatment in their own country. Services of long-term care (LTC) to support people in their activities of daily living (ADL), organ transplants and national vaccination campaigns are excluded.
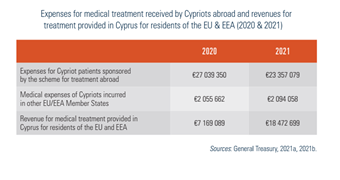
The patient, prior to their departure from the Republic of Cyprus for cross-border health care in another Member State, is required to submit a request for prior authorization to the National Contact Point. Prior approval can be rejected in the following cases: a) the patient will be exposed to a patient safety risk; b) the public will be exposed to a substantial safety hazard as a result of cross-border health care; c) the health care is to be provided by a provider that raises serious and specific concerns relating to standards and guidelines on quality and patient safety; d) the health care can be provided on its territory within a time limit which is medically justifiable, taking into account the current state of health and the probable course of the illness of each patient concerned. In 2021, the medical expenses of Cypriots incurred in other EU/EEA Member States came to just over €2 million (Table2.5).
Table2.5
For health care services that are not provided in Cyprus, the MoH also implements a sponsored patient scheme for treatment abroad. The scheme concerns mainly positron emission tomography (PET) scan examinations, transplants and specialized paediatric cases, and, in 2021, dispersed just over €23 million in sponsorship. The countries to which they are sent for treatment are primarily Greece, Germany and the United Kingdom. The MoH also records the revenues from medical treatments provided in Cyprus for residents of other EU/EEA Member States. The total amount for 2020 was €7 169 089, which increased to €18 422 699 in 2021 (General Treasury, 2021a, 2021b).
The Health Insurance Organization (HIO) has introduced a structural reform regarding the management of patients sent abroad for healthcare services. This reform represents a significant revision of the governance and operational framework for cross-border healthcare within the GHS (ΓεΣΥ), aiming to streamline processes, enhance clarity and ensure efficient management of cases requiring treatment abroad.
As of 2 October 2025, the HIO is responsible for processing and approving all overseas referral requests for GHS beneficiaries when the required medical service falls within the GHS benefits package and cannot be provided in Cyprus due to limitations in expertise, technology or clinical conditions. Requests for non-GHS beneficiaries will continue to be managed centrally by the Ministry of Health.
The HIO has also clarified that certain categories of services do not fall under its responsibility. These include interventions not sufficiently tested or recognized by conventional medicine, treatments in an experimental stage, requests relating solely to drug administration, non-conventional medical practices, telemedicine services and retroactive requests for services already received. Applications in these categories will continue to be overseen and processed by the Ministry of Health.
To ensure timely processing, the HIO has introduced a classification system with specified assessment timelines. Regular cases—those without strict time constraints—are evaluated within 15 days. Urgent cases, requiring accelerated management, are processed within 7 days, with the HIO typically completing assessments within 4 days. Life-threatening cases, requiring immediate attention, are processed within 2 days, with evaluations usually finalized within 24 hours.
The HIO has established a list of collaborating international hospitals for the provision of approved services abroad. However, beneficiaries retain the right to select a hospital outside this list. In such cases, and upon approval of the request, the beneficiary and their treating physician must make all necessary arrangements related to scheduling and admission. Coverage remains subject to the terms of the approved referral.
More information: Health Insurance Organization Announcement (in Greek).