-
29 July 2025 | Policy Analysis
Spain creates a National Public Health Agency to strengthen public health governance -
20 March 2025 | Country Update
Draft law to prevent underage drinking -
01 July 2024 | Country Update
Improving capacities in Public Health Surveillance -
05 April 2024 | Country Update
Expanding smoking reduction policies
5.1. Public health
On 11 March 2025, the Council of Ministers approved referring the draft law for the prevention of consumption of alcoholic drinks by underage persons to the parliament. Beyond preventing alcohol consumption and protecting young people from its effects, the law also aims to create safe and healthy environments and provide health promotion workers with effective tools to stimulate healthy habits.
Among other measures, alcohol consumption will be prohibited in places where minors are a majority, such as educational and sports centres. The sale and display of alcoholic beverages will be forbidden in establishments that are primarily intended for underage persons. The regulation also prohibits advertising alcohol beverages to minors or minimizing health risks in advertising aimed at the general population. It also forbids commercial alcohol-related communication on public roads within a 150-metre radius of educational, health and social centres, parks and playgrounds.
More information (in Spanish): https://www.sanidad.gob.es/gabinete/notasPrensa.do?id=6635
References
More information (in Spanish):
Royal Decree 568/2024 of 18 June creating the State Public Health Surveillance Network https://www.boe.es/buscar/act.php?id=BOE-A-2024-12379
Public Health Strategy https://www.sanidad.gob.es/ciudadanos/pdf/Estrategia_de_Salud_Publica_2022___Pendiente_de_NIPO.pdf
The Plan comprises five main goals: preventing smoking initiation, promoting smoking cessation, reducing environmental exposure to tobacco (and related products), supporting applied research on tobacco control, and enhancing coordination and partnership building.
The specific measures of the Plan will be implemented by developing different laws whose scope will be: equating new tobacco products (for example, vaping) to traditional tobacco when it comes to production and advertising; implementing plain tobacco packaging; increasing smoking-free areas; expanding tobacco cessation programs; and transposing European regulations on this area; and implementing new taxation policies.
The Ministry of Health has committed to fund part of these measures through an increase in the tobacco excise taxes.
References
Press release Ministry of Health (in Spanish) https://www.sanidad.gob.es/gabinete/notasPrensa.do?id=6387
2024–2027 Prevention and Control of Smoking Plan 2024–2027 (in Spanish) https://www.asomega.es/wp-content/uploads/PIT_R5_05_2024.pdf
5.1.1. Public health institutions and authorities
Competences in public health planning and provision were transferred to the 17 ACs and the two autonomous cities of Ceuta and Melilla between 1979 and 1981 (see section 2.3 Decentralization and centralization). Public health within ACs has a dedicated structure where a public health authority, usually a General Directorate within the Health Department, a) ensures the enforcement of the regulations passed to support public health policies; b) holds the executive planning role for operational public health services; c) coordinates population-based programmes (such as vaccination or cancer screening programmes); and d) monitors the health status, health determinants and health risks of the population residing in the AC.
Beyond the monitoring and surveillance activities provided within the public health structure, the SNS PHC doctors and nurses are the core public health agents; they represent the main workforce in the deployment of population-based programmes, although they are mainly focused on prevention programmes (infant and older people vaccination programmes, primary and secondary prevention of noncommunicable diseases, opportunistic screening activities, counselling activities).
Other relevant public health agents are teachers and NGOs, who work as mediators in the implementation of prevention and health promotion programmes, as well as municipalities, as critical actors in the actual provision of sanitation and environmental protection and, in larger cities, in food safety control, animal slaughter regulation and local health promotion programmes (such as healthy cities networks).
Besides the public health activities developed at regional level, the Ministry of Health, through the General Directorate of Public Health, holds responsibility for certain public health tasks such as international health activities, international movement of commodities and passengers, food safety regulation, the system of alerts for health emergencies and, notably, the coordination of the 17 public health units of the ACs’ Departments of Health and INGESA (see section 2.2 Organization). This coordination usually takes place within the CISNS, particularly throughout the working groups that compose the Public Health Commission, where public health strategies are agreed, ensuring cohesion and quality across the country.
Context
Spain’s public health governance was significantly challenged during the COVID-19 pandemic, revealing the need for a stronger institutional framework to manage health surveillance, intersectoral coordination, risk assessment and crisis preparedness. Until now, responsibilities were fragmented across various entities with limited coordination. Notably, the creation of a National Public Health Agency was a provision in the 2011 General Law of Public Health that was pending implementation.
Impetus for the reform
In the aftermath of the pandemic, a parliamentary special committee on the Social and Economic Reconstruction of the country, as well as the commissioned Evaluation on the Spanish health system response, recommended strengthening public health institutions and procedures, recognizing some weaknesses of the system and providing recommendations for enhanced responsiveness. Recommendation translated into specific funding as part of the EU Recovery and Resilience Plan.
Main purpose of the reform
The Law 7/2025, of 28 July, creates the National Public Health Agency (Agencia Estatal de Salud Pública, AESAP), an independent public agency attached to the Ministry of Health, to reinforce the protection of population health. The AESAP assumes technical responsibilities previously held by the Ministry of Health, making technical and scientific recommendations in surveillance and assessment of the health status of the population. The authority remains in the Ministry of Health in coordination with the ACs. The reform also entails increased infrastructure and human resources to accomplish these functions.
Content/characteristics
The AESAP assumes technical responsibilities previously held by the Ministry of Health, in coordination with the ACs, encompassing the surveillance, identification and assessment of the health status of the population. It is responsible for public communication on health risks, coordination of crisis preparedness and emergency response, and technical cooperation with regional public health services.
It also supports public administrations and civil society on health promotion, disease prevention, and addressing social determinants of health. The AESAP will participate in the design and evaluation of public health policies and promote research, training and innovation. It will also coordinate the State Network for Public Health Surveillance, and will assess health outcomes related to health services (in collaboration with ACs). These roles reinforce the state’s public health capacities without undermining regional competences.
Law 7/2025 also grants to the AESAP the authority to access and manage health data from ACs and other sources, reinforcing its legal capacity to collect and analyze public health information. This requires technical interoperability across the health information systems of the ACs and a new governance model for data sharing between administrations.
Implementation steps taken (or scheduled)
The law entered into force on 30 July 2025. Within six months, a royal decree will approve the AESAP’s statute, define its governance, and transfer relevant services and staff from the Ministry of Health, for example, those related to health alerts and emergency response or health policy evaluation. Coordination with ACs is foreseen via the Interterritorial Council, and a multilevel governance model is expected to be facilitated, pending the drafting and approval of the AESAP’s statute, through mechanisms for cooperation, data sharing and the promotion of collective intelligence.
Outcomes to date and any evaluation
As of July 2025, the reform has been enacted, and preparatory steps for implementation are underway. The forthcoming framework agreement between the Ministry of Health and the AESAP will establish mechanisms to assess accountability and performance.
References
Law 7/2025, of 28 July, establishing the State Agency for Public Health (https://www.boe.es/boe/dias/2025/07/29/pdfs/BOE-A-2025-15652.pdf)
Law 33/2011, of 4 October, General Law on Public Health (https://www.boe.es/buscar/pdf/2011/BOE-A-2011-15623-consolidado.pdf)
Report of the Commission for Social and Economic Reconstruction 2020 (https://www.congreso.es/docu/comisiones/reconstruccion/153_1_Dictamen.pdf)
EVALUACOVID-19: Evaluation of the performance of the Spanish national health system in the COVID-19 pandemic (https://www.sanidad.gob.es/areas/alertasEmergenciasSanitarias/alertasActuales/nCov/documentos/EVALUACION_DEL_DESEMPENO_DEL_SNS_ESPANOL_FRENTE_A_LA_PANDEMIA_DE_COVID-19.pdf)
Recovery, Transformation and Resilience Plan (Component 18, Reform 2) (https://www.lamoncloa.gob.es/temas/fondos-recuperacion/Documents/05052021-Componente18.pdf)
5.1.2. Public health strategies
An important milestone was the publication of Law 33/2011 on Public Health, which issued the principles and actions to include “Health in All Policies” in institutional actions on health, and sought to update and upgrade the coordination mechanisms amongst the 17 AC Departments of Health and INGESA, essentially in terms of epidemic surveillance and control, and the provision of common benefits: namely, a common vaccination calendar, common neonatal screening tests and cancer screening. Some elements, such as the creation of a National Agency for Public Health, have recently been approved as a draft law (see section 6.2 Future developments).
Importantly, the reflection process following the COVID-19 pandemic prompted the publication of the national public health strategy (Ministry of Health, 2022b), creating a reference framework for the coordination of all the actors involved in public health. In addition, the Strategy has been thought of as an instrument that efficiently articulates and links the different public health initiatives developed at international level, translating actions into national, regional and local policies. Main strategic lines are strengthening public health to improve the health of the population; modernizing public health surveillance and ensuring preparedness to respond to health risks and emergencies; improving health and well-being through the promotion of healthy, safe and sustainable lifestyles and environments; and promoting health and health equity throughout the life-course.
In the specific case of public health surveillance, the Strategy aims to leverage health information in a timely manner, since the COVID-19 pandemic revealed weaknesses and structural failures in surveillance. The general objective is to set up a flexible, homogeneously developed National Surveillance Network in the SNS. The Network will collect, analyse, interpret and disseminate information about health population status, health determinants and public health risks, generating knowledge to reinforce preparedness, to support decision-making and to evaluate public health actions. The Strategy has 30 objectives grouped into seven strategic lines, notably the development of a workforce policy to guarantee the quality and effectiveness of public health surveillance, an authoritative role for public health surveillance in decision-making, and a new governance framework for public health surveillance based on a National Network, where hubs are the general directorates of public health in the ACs.
5.1.3. Immunization
In 2021 and 2022, the effective implementation of the COVID-19 vaccination programme was notable, with Spain being one of the leading countries in terms of timely coverage; for example, Spain was the first country to vaccinate 100% of the population aged 80 and older and reached high vaccination coverage rates in people over 12 years of age with a complete vaccination schedule. More than 39.1 million inhabitants, or 92.8% of the population, were vaccinated. Furthermore, 80% of people aged 40 and older were covered with a booster (Ministry of Health, 2022f).
Other public health programmes remain active since their introduction over the last decades. Coverage of vaccination programmes for children remains high and stable over time: in 2022, a 95% coverage rate was seen for primo-vaccination in polio, DTaP, triple viral, pneumococcal and meningococcal vaccines, while a 91% coverage rate has been reached for the chickenpox (Varicella) vaccine (Ministry of Health, 2023p). In 2022, flu vaccination in people aged 65 and over had a 68.6% coverage rate, mainly due to the combination of both flu and COVID-19 annual vaccination campaigns (Ministry of Health, 2023a).
5.1.4. Screening programmes
The Health Departments of ACs are responsible for the executive coordination of population-based screening programmes. Regarding cancer screening, there has been an increase in coverage, which has been particularly high in the case of colorectal cancer. Coverage for population-based breast cancer screening programmes has slightly increased over time, from 75.2% in 2015 to 81.9% in 2020 (Ministry of Health, 2023a). The population-based screening programme for colorectal cancer has witnessed a sharp increase; faecal occult blood tests covered 32% of the target population in 2020 (12.4% in 2014) similarly for both men and women (Ministry of Health, 2020b). Pap-smear tests have remained stable, above 70% of the eligible population, since 2014. However, coverage is greater in the better-off (higher income) populations: 6% higher for breast cancer and colorectal cancer screenings, and 10% higher for cervical cancer (2017 data). Differences across ACs are also notable (Ministry of Health, 2023r; Ministry of Health, 2020b).
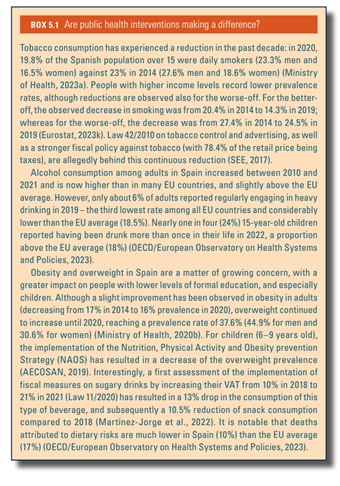
Box5.1 assesses the effectiveness of public health interventions, focusing on those that address tobacco and alcohol consumption, and obesity and overweight.
Box5.1