-
21 September 2024 | Country Update
Regulation on cosmetic surgery
4.2. Human resources
In recent years in Spain, the number of surgical interventions for aesthetic purposes (those not included in the benefits basket) as well as the number of private health centres offering cosmetic surgery, has increased significantly. The proliferation of this kind of centres has generated a growing demand for better regulation of its activity. In this context, the Ministry of Health published an Order on 21 September amending the previous Royal Decree 1277/2003, which establishes the bases for the authorization of health centres, services and establishments.
The new Order aims to restrict the performance of cosmetic surgery procedures to only those healthcare professionals passing the residency program for Plastic, Aesthetic and Reconstructive Surgery or another surgical or medical-surgical specialization that includes competencies in aesthetic surgery.
References
Order SND/1002/2024, of 18 September, amending Annex II of Royal Decree 1277/2003, which establishes the general bases for the authorization of health centres, services and establishments (https://www.boe.es/diario_boe/txt.php?id=BOE-A-2024-18934)
Royal Decree 1277/2003, of 10 October, which establishes the general bases for the authorization of health centres, services and establishments (https://www.boe.es/buscar/act.php?id=BOE-A-2003-19572&b=17&tn=1&p=20240921#anii)
4.2.1. Planning and registration of human resources
There has been a substantial increase in the number of medical schools in Spain, from 28 in 2010 to 53 in 2023 (public and private), offering a total of 7519 places in that year (Ministry of Science, Innovation and Universities, 2023). Nevertheless, there were 6316 graduates in medicine in 2023, the lowest number since 2016, and below the European Regional average (15.3 graduates per 100 000 population) (Barber-Pérez & González López-Valcárcel, 2022; WHO Regional Office for Europe, 2022b).
Specifically, in order to increase the number of graduate physicians, 706 new places for medicine degrees at public universities were offered in the academic year 2023–2024, reaching a total of 6106 places in the first-year course. Public universities received €52 million from the Spanish Government to support this increase (Royal Decree 698/2023).
In any case, the number of new graduates did not match the number of vacancies in the Medical Internship Programme (known as “MIR”), the nationwide specialization programme that establishes a doctor’s entitlement to practise in the SNS (for example, in 2023 there were 8772 vacancies, Order SND/990/2023).
This mismatch between new graduates and the offer of specialist training places, which exists concurrently with an unbalanced replacement rate (for example, 60% of the family doctors are over 50 years of age) may lead (if it has not already) to a shortage of medical doctors for some specialties.
In order to foresee an appropriate number of physicians for each specialization according to unmet needs, the Ministry of Health periodically orders a report assessing the supply and demand of medical specialties. The report aims to help inform decision-making about variables affecting physician availability: age of retirement, number of Medical Internship vacancies or the overall Medicine University quote.
The latest report published in January 2022 (Barber-Pérez & González López-Valcárcel, 2022) stated that in 2021 the specialties with the largest deficits were: family medicine (with the highest predicted shortage in 2027), anaesthesiology, geriatrics, psychiatry and radiology (the reference point to determine the gaps was a 2021 expert survey assessing needs at the time). In a predictive model on mid-term needs, these specialties also forecast deficits in covering needs in 2028. On the other hand, clinical analysis, cardiac surgery and internal medicine were the specialties with the largest surplus in 2021. Regarding the future needs of the health system, based on country demographics and need ratios, the report’s authors concluded that long-term needs for physicians would increase by 9% in 2035. In addition, as a sharp increase in the ageing population (particularly those aged 80 and over) is expected in the upcoming years, the SNS would need more physicians treating chronic and multimorbid patients (primary care and internal medicine) and fewer paediatricians. Based on this evidence, the Inter-territorial Council mandated the Spanish Ministry of Health to increase the number of positions for the Medical Internship Programme. Consequently, since 2019 there has been a significant growth in the number of positions, from 6797 vacant positions to cover in the 2019 call to 8772 in the 2024 call (29% increase) (AMIR, 2024). Likewise, the number of positions for training in the six nursing specialties has also increased – even more than in the case of physicians, from 1092 nurse training vacancies to cover in the 2019 call, to 2108 in the 2024 call (93% increase) (Order SND/990/2023).
Registration, licensing and access to specialization of health professionals in Spain are regulated by the Health professions organization Law (Law 44/2003). Since 2003, there have been very few changes to the registration and licensing requirements set out in the legal text.
4.2.2. Trends in the health workforce
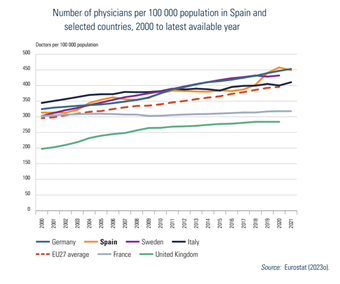
Relative to the averages in the EU, Spain has a higher density of doctors and a lower density of nurses (Fig4.2). As Fig4.3 shows, the number of practising medical doctors in Spain is significantly above the EU average and follows the same growing trend as in other EU countries. Thus, from 380 active physicians per 100 000 inhabitants in 2014, the number has increased, reaching 449 in 2021. The largest increase was in the period from 2018 to 2019 (402 to 440). The EU average ranged from 302 active physicians per 100 000 population in 2015 to 325 in 2021 (Eurostat, 2023m).
| Fig4.2 | Fig4.3 |
 |  |
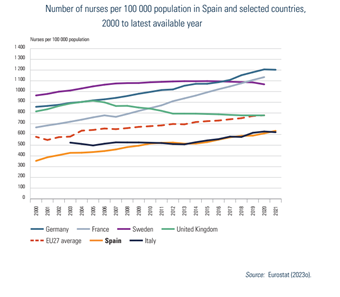
In contrast, in the case of nurses, the rate in Spain remains below the EU average (Fig4.4). In 2021, there were 634 nurses per 100 000 inhabitants in Spain, whereas the EU average in 2020 was 779 (Eurostat, 2023m). The ratio of nurses to doctors in 2021 was 1.41, below the EU average of nearly 2 (1.97) (Eurostat, 2023m).[15]
Fig4.4
The primary care workforce remained constant throughout the period 2014–2022, ranging between 76 and 78 primary care physicians (family doctors) per 100 000 assigned population and from 65 to 70 per 100 000 assigned population in the case of PHC nurses. In contrast, the number of specialized care staff has increased in recent years: the number of specialist physicians working in hospitals and outpatient specialized settings has increased from 181 per 100 000 inhabitants in 2014 to 214 in 2022. Similarly, staff nurses working in hospitals and outpatient specialized premises rose from 314 to 387 nurses per 100 000 inhabitants in the period 2014–2022 (Ministry of Health, 2023a).
Health care staff in Spain are older than the European average. Specifically, in 2020, 32% of doctors are over 55 years old in Spain, whereas this percentage is 30.1% in Europe. In the case of nurses, in Spain 20.9% are over 55 years old, while in Europe this percentage is 18% (WHO Regional Office for Europe, 2022b).
From a gender perspective, the number of women accessing staff positions as physicians has continued to grow, from 52.6% in 2015 to 57.6% in 2021, which is above the European average of 52% (Eurostat, 2023n). In public centres, the figure reaches 61% of physicians. The number of women accessing staff positions has varied according to the workplace; in 2020, 62% of PHC physicians were women (11 percentage points more than in 2010, and 6 percentage points more than in 2015), but in the case of hospitals and outpatient specialized settings, the share of women remained slightly lower (55% of medical staff in 2020), although improving on 2015 figures, with a 5.3 percentage points increase. However, the gender gap remains as women are not reaching leadership positions in health care, professional organizations, academic positions and research. For example, just 26% of women held the position of head of department at medical universities in the academic year 2020–2021 (Santucci et al., 2023).
In the case of dentists, although there are some working as salaried staff in primary care settings, most are private providers that generally work in small practices and increasingly as salaried workers in franchising companies. From 2010 to 2020 there has been a 43% increase in the number of dentists. In 2020, the average ratio of inhabitants per dentist was 1192, with Madrid showing the lowest number at 778 inhabitants per dentist and Castile-La Mancha the highest across regions at 2021 inhabitants per dentist (General Council of Dentists, 2022).
In the case of pharmacists, in 2022 there were 79 288 registered pharmacists in Spain, with 71.9% of them being women. Around 56 502 pharmacists (71%) worked at community pharmacies that year: 45% of them were owners of community pharmacies, whereas 44.2% worked as assistant pharmacists. Spain has one of the highest rates of pharmacists in the EU, with 126 pharmacists per 100 000 inhabitants in 2021, showing a 5% increase from 2015 to 2021 (Eurostat, 2023m). The variation in the rate of pharmacists across ACs in 2022 ranged from 123 per 100 000 inhabitants in the Balearic Islands to 232 per 100 000 inhabitants in Navarre (General Council of the Official College of Pharmacists, 2023).
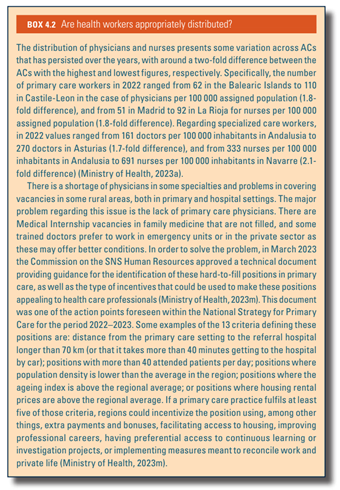
Box4.2 assesses the distribution of health workers in Spain.
Box4.2
- 15. This relatively lower nurses’ density is influenced by the fact that Spain does not report nurse assistants (or nursing aides) in the statistics. This constitutes a large category of workers in the SNS. Midwives are included in the ratio. ↰
4.2.3. Professional mobility of health workers
Spain is a net importer of doctors, and together with Germany and the United Kingdom was one of the main countries of destination in absolute terms for foreign-trained doctors and nurses in 2020 (WHO Regional Office for Europe, 2022b). The immigration of non-specialist doctors, who mainly come from Latin America, correlates with the economic cycle and with public spending on health. In that regard, until 2019 there has been a continuous increase in the number of doctors trained in foreign countries, when 6354 physicians entered Spain to work. The decrease observed during the COVID-19 pandemic was overcome in 2021 with an inflow of 4293 qualified medicine graduates (Barber-Pérez & González López-Valcárcel, 2022). There is a high demand in the private sector for these non-specialist doctors. Speeding up the official recognition of medical degrees has become a policy instrument for workforce management when the SNS is suffering from some extreme shortage (Barber Pérez & González López-Valcárcel, 2024).
When it comes to outflows, in the aftermath of the economic crisis (after 2012) the number of physicians requesting the “certificate of good standing” required to work in other EU countries increased from 2405 in 2012 to 4100 in 2019. In 2020, requests decreased to 3559. However, many doctors ask for more than one competence certificate (they are different for each country), and in many cases they do not move to another country, so the actual number of Spanish doctors arriving in other countries is lower (Barber-Pérez & González López-Valcárcel, 2022). According to OECD figures, in 2020, 204 new Spanish physicians enlarged the number of doctors working in foreign countries (Barber-Pérez & González López-Valcárcel, 2022). The usual destinations for doctors have been the United Kingdom, France, Germany, Ireland and Belgium. When it comes to family doctors, the underlying reasons for this outflow are insufficient salary, job insecurity and time frames of contracts, excessive workload, poor primary care governance and lack of flexibility (Calderón-Larrañaga et al., 2024).
Similar behaviour was observed in the case of nurses; between 2010 and 2013, 4580 nurses requested the “certificate of good standing” from the Ministry of Education; in 2014, 8000 nurses were working abroad (Galbany-Estragués & Nelson, 2016), while in 2022 the number reached approximately 1100 nurses. In this case, the main destinations have been Norway, the United Kingdom and Ireland (General Council of Nurses, 2023).
4.2.4. Training of health personnel
In 2022, 31 293 medical doctors were trained within the medical residents’ programmes. The specialty of Family and Community Medicine was the specialty for most residents in training (8477 residents, 27.1% of the total), followed by paediatrics (1909) and internal medicine (1758). Likewise, Family and Community Nursing was the nursing specialty for most nurses in training (1416 in 2022, 42%), followed by obstetric gynaecological nursing (865, 26%) and mental health nursing (486, 14%) (Ministry of Health, 2023o).
On a different note, prompted by the Recovery, Transformation and Resilience Plan, the Ministry of Health and the Ministry of Universities promoted in 2022 the requirements and procedures for the inclusion of new specialties in health sciences (medical and nursing internship programmes) (Royal Decree 589/2022). The first new specialty proposed under this new regulation is the title of specialist in Emergency and Emergency Medicine (Royal Decree 610/2024).
4.2.5. Physicians’ career paths
Physician careers, regulated in Article 38 in Law 44/2003, have not changed in recent years. The upgrading mechanisms foreseen in this Law, and which entail salary supplements or training benefits, are dependent on ACs’ policies, which may translate into differences across regions.
The large increase of temporary workers in the public sector over the years (from 28.5% in 2012 to 41.9% in 2020) (Hernández Pascual & Cabezón Rodríguez, 2022) has prompted some reforms to improve job stability. Hence, from July 2022, temporary contracts in the SNS must be limited to a maximum of three years’ duration and are restricted to specific situations (for example, health programmes) or to cover long-run vacancies. In the case of need for the specific post to remain, health authorities are obliged to create a permanent position in the corresponding health care provider (Royal Decree-Law 12/2022). In the specific case of primary care, the objective is to reduce the share of temporary contracts below 8% (Ministry of Health, 2021d).
4.2.6. Other health workers’ career paths
As in the case of doctors, other health workers’ careers are regulated in Article 38 in Law 44/2003 and no changes have been observed since the last HiT report except the implementation of policies improving job stability.
Notably, an important achievement in nursing has been the approval of nursing prescriptions. Since October 2018, nurses are entitled to decide on the medicine indication, and utilize and provide prescription drugs, subject to the existence of protocols and clinical guidelines that should specify in which cases prior medical validation is needed. Additionally, nurses can prescribe the vaccines included in the official vaccination calendar or those related to specific vaccination campaigns. To prescribe, staff nurses are required to obtain a certification demonstrating professional experience or having passed a specific training programme (Royal Decree 1302/2018).