-
09 February 2023 | Country Update
Piloting of a complex care programme for patients with Parkinson’s Disease to start in 2023 -
02 December 2022 | Country Update
Introduction of care coordination within primary health care
5.2. Patient pathways
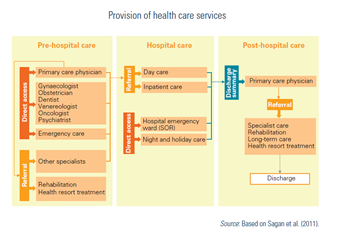
Patient pathways in the statutory health system are similar across the country and for everybody, except for patients with suspected cancer and other patients who are covered by coordinated/integrated care models (see Box5.3 and Table5.2). A typical pathway will depend on the urgency of care. If immediate care is needed, patients can access emergency care directly (without a referral; see Fig5.3), in both ambulatory setting (within “night and holiday care”) and, for more serious problems, in the SOR, irrespective of their insurance status. However, after the patient has been stabilized, uninsured persons may be required to cover the cost of subsequent care out of their pocket.
| Box5.3 | Table5.2 |
 |  |
Fig5.3
In case of non-urgent care, a patient’s journey usually begins with a visit to their “first-contact physician” (typically a GP/family physician or a paediatrician in case of children). Patients can enrol with any PHC physician who has signed a contract with the NFZ. There are no territorial restrictions in the choice of GP, such as place of residence. Patients can switch to a different PHC physician free of charge up to two times during the calendar year. For each subsequent change a fee of PLN 80 is due. This fee is waived if patients switch their GP because of the change of the place of residence; if their previous GP ceases to provide services; or for any other reason for which their previous GP was responsible. The PHC physician should be able to help with common health issues. If a specialist treatment is needed, the PHC physician will refer the patient to a diagnostic examination or a specialist doctor and/or hospital. In future, according to the 2017 Act on Primary Health Care, a PHC physician will also be responsible for coordinating the entire process of treatment (see section 5.3). There is no need to have a referral to see the following specialists: gynaecologist and obstetrician, oncologist, psychiatrist, venereologist and dentist (until the end of 2014, referrals were also not required for consultations with a dermatologist or ophthalmologist). Certain population groups are exempted from having to have a referral to access outpatient specialist care.[14] All care provided by PHC physician and all specialist care with a referral is free of charge as long as the health care provider has a contract with the NFZ. Prescribed outpatient medicines may be subject to cost-sharing but all medicines received as inpatients are free of charge (see section 3.4).
A referral will usually remain valid until it is actually used (there is no time limit).[15] Patients can freely choose among all specialist service providers (public or private) that have a valid contract with the NFZ – the exception to this are coordinated care programmes (see Box5.3 and section 5.3). Once they have chosen the provider, they have to register with them (they can only register with one provider – this also applies to services that do not require a referral and oncological services) and are entered onto a waiting list. The patient has access to the publicly available information on the waiting times in individual hospitals (through their websites and through a dedicated website; see Table2.4). The date of appointments can only be brought forward due to medical considerations. If the patient does not want to wait for the procedure, they can have it done at a non-contracted private or public provider and pay for it out of pocket.
Table2.4
If additional diagnostic examinations are required, a referral will be issued by the specialist attending the patient. If the patient fails to come to the appointment, unless this has been caused by a force majeure, they will be deleted from the waiting list. After specialist treatment has been completed the patient is discharged and receives a discharge summary that describes the treatment she/he received and recommendations for further care. If necessary, the PHC physician refers the patient for further care. Referrals for health resort treatment are submitted to the voivodeship branch of the NFZ where decisions are made concerning the necessity of treatment, its setting (health resort hospital, sanatorium, spa outpatient clinic), type of therapy as well as its duration.
- 14. The following population groups can access outpatient specialist care without a referral: war invalids and persecuted persons, combatants, anti-communist opposition activists and people repressed for political reasons, and civilian blind victims of war; persons with addictions to alcohol and narcotic drugs or psychotropic substances(for addiction treatment, this includes persons in a relationship with an addict); soldiers or civil servants (for treatment of injuries or illnesses incurred while on duty outside the country); war veterans (for treatment of injuries or illnesses incurred while on duty outside the country); children under 18 suffering from congenital diseases diagnosed in prenatal tests; persons with tuberculosis; HIV-positive patients. ↰
- 15. Exceptions include referrals for health resort treatment (which are verified every 18 months from the date they are issued and become invalid if the verifying physician asserts that the patient is no longer in the need of such treatment); referrals to outpatient physiotherapeutic procedures (they become invalid if the patient is not registered at the rehabilitation institution within 30 days from the date referral was issued); referral to a psychiatric hospital (they become invalid after 14 days). ↰
Approximately 100 000 people suffer from the Parkinson’s Disease in
Poland, and this number is expected to rise in the coming years. The
therapy for this disease requires a multidisciplinary approach, with
cooperation between neurologists, family
doctors, but also other specialists, such as radiologists,
physiotherapists, psychologists, speech therapists, dietitians,
gastroenterologists and others. While the availability of medical
treatment options has been increasing, appropriate specialist
supervision of further specialist treatment is not always
available.
To that end, a programme of complex care for patients with Parkinson’s Disease is likely to be piloted from 2023 in three centres – in Gdańsk, Warsaw and Wrocław. This model was developed in 2018, but has not been introduced so far.
For more information (in Polish) see:
Authors
New regulations of the Ministry of Health, in force since 1 October 2022, introduced care coordination within primary health care. This will cover diagnosis and treatment in four disease areas that are most frequently diagnosed within PHC:
- Cardiology (arterial hypertension, heart failure, chronic ischemic heart disease and atrial fibrillation)
- Diabetology (diabetes mellitus)
- Pulmonology (bronchial asthma and chronic obstructive pulmonary disease)
- Endocrinology (hypothyroidism and diagnosis of nodules of the thyroid gland)
Participation of PHC doctors in care coordination is voluntary. Those who decide to offer coordinated care will be able to refer patients to comprehensive (mainly laboratory) diagnostic tests related to the four disease areas above and consult with cardiologists, diabetologists, pulmonologists, allergists, and endocrinologists, within PHC, without referring patients to these specialists. PHC nurses will be involved in patient education and patients will also be able to consult a dietician.
These changes are expected to improve detection and diagnosis of the most common chronic diseases and facilitate comprehensive patient care within PHC. They implement some of the solution tested within the PHC pilot between 2018 and 2021 (see Policy Analysis from 10 October 2021).