-
03 December 2025 | Country Update
Creation of a National Procurement and Logistics Centre
7.6. Health system efficiency
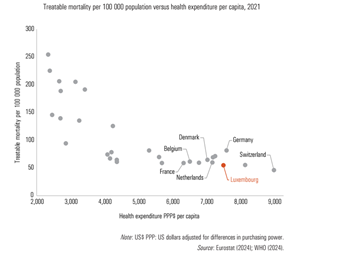
Health system efficiency involves maximizing desired outcomes while ensuring optimal allocation of resources (Cylus, Papanicolas & Smith, 2016). A cursory illustration of the health system’s performance in terms of input costs and outcomes can be obtained by plotting CHE against the treatable mortality rate. At this very macro level, Luxembourg shows one of the lowest treatable mortality rates per 100 000 population in Europe (see section 7.5), yet, it also has one of the highest per capita expenditures. Countries with comparable treatable mortality rates, such as the Netherlands, France and Belgium (see Fig7.6), maintain considerably lower health expenditure per capita. This suggests that there is room for improvement in terms of this basic efficiency metric.
Fig7.6
A law adopted on 3 December 2025 establishes the National Procurement and Logistics Centre (Centrale nationale d'achat et de logistique, CNAL) which will centralize and coordinate purchasing and logistics of medical products for many inpatient and outpatient providers. It operates under the supervision of the Minister of Health and is funded through an annual allocation and contribution from the state budget.
The new centre aims to enhance organizational efficiency, reduce administrative workload for health and pharmaceutical staff, generate budget savings, and optimize storage capacities. Centralizing procurement is also intended to strengthen the national health system’s responsiveness and improve availability of essential medical supplies.
The centre’s responsibilities include:
- operating as an external hospital pharmacy under the supervision of a responsible pharmacist;
- procuring, storing and distributing medical and sanitary products, medicines and related supplies;
- establishing, managing and maintaining the national critical and strategic stock, including vaccines and personal protective equipment; and
- procurement and distribution of medicines for the national immunization programme.
7.6.1. Allocative efficiency
Mechanisms for priority setting in budget allocation are absent and the use of evidence regarding effectiveness and cost-effectiveness is limited (see sections 2.7.2, 2.7.3 and 3.3.3). The risk-adjusted resource allocation is not used. This can be explained by the positive financial situation of the SHI for several years, making priority setting from a health spending perspective optional. Consequently, prevention and health promotion are underdeveloped, and overuse for some types of care has been observed.
Specifically, there is an apparent pattern of excessive CT and MRI examinations. When considering both types of examinations, Luxembourg ranks among the countries with the highest number of CT and MRI scans within the OECD in 2021, totalling 360 examinations per 1000 population, surpassed only by the United States of America and the Republic of Korea, which report 362 examinations per 1000 population. This rate significantly exceeds the OECD average of 249 examinations per 1000 population (OECD, 2023). Efforts to address the excessive use of diagnostic examinations were implemented through a national plan, which included actions such as regulation, education and training, guidelines, and audits. Audits conducted in 2016 and 2023 showed a slight improvement in the rate of justified MRI examinations from 78% to 80% and a notable improvement from 61% to 75% for CT examinations (Bouëtté et al., 2019) (see section 4.1.2).
In response to Luxembourg’s high caesarean section rate, which averaged 32% from 2014 to 2016, health professionals developed reduction measures. This included publishing an informative brochure for parents and national recommendations on scheduled caesareans. An assessment in January 2020 confirmed that these efforts had been successful, as the rate dropped below 30% for the first time in many years, though improvements are still needed for caesarean sections on multiparous women with a previous caesarean (Weber et al., 2022).
Although prevention is highlighted as a priority in both the National Health Plan 2023 and the government programme for 2023–2028, its implementation in Luxembourg remains negligible. Notably, a national prevention or health promotion strategy is absent. While some programmes (for example, breast cancer screening) and specific medical procedures (for example, dental examinations during pregnancy and early childhood) exist (see sections 3.7.1 and 5.1), prevention is not included in the SHI benefit package (CSS Art. 17). Consequently, health care providers lack incentives to engage patients in discussions about healthy behaviours or encourage regular health check-ups. The current system fails to effectively promote a healthy lifestyle (see section 7.5).
7.6.2. Technical efficiency
p>The financing system for hospitals in Luxembourg does not incentivize efficiency improvements, as made evident by the notably higher average length of hospital stays compared with the EU average and the low bed occupancy rate. The hospital financing mechanism operates on a resource-oriented rather than a results-driven approach. Additionally, the reimbursement system for the services of predominantly autonomous physicians operates independently from the hospital-financing framework, and medical procedures are reimbursed retroactively by SHI. The hospital therefore has limited capacity to steer activity (Rausch, 2021). Physicians get paid the same whether they are treating a patient in a hospital, in an ambulatory, or a day care setting. In an inpatient care setting, physicians have the possibility to charge convenience fees (see section 3.4). There is no pay-for-performance system. All services, including hospital services, are remunerated on an FFS basis (see section 3.7). However, Luxembourg has shown improvement in the technical efficiency of its hospital sector over the recent years (2017–2021). There has been a notable rise in day-case surgery rates, increasing from 41.6% of all hospital admissions in 2017 to 48.1% in 2021. Although Luxembourg’s rate for cataract surgeries now surpasses the OECD average of 93.8%, its rate for tonsillectomies remains below the OECD average of 40.0% (OECD, 2023). The average length of stay for inpatient hospitalizations remained stable at 7.3 days between 2012 and 2021. The stable average length of stay can be explained by the fact that short stays are increasingly managed as day hospitalizations and thus excluded from this calculation. In 2021, the average stay for acute care was 5.6 days in France, 6.3 days in Belgium and 7.4 days in Germany (ObSanté, 2024). In 2023, the shortage of rehabilitative care beds was addressed by increasing their number, aiming to reduce the number of delayed discharges for acute care, which should influence the average length of stay in the longer term.
For a long time, there have been discussions and efforts to foster the pooling of activities in the hospital sector, such as information technology, laboratories and joint purchasing. The 2010 Health Reform envisaged the centralization of these hospital activities. While efforts in this direction have been undertaken by the FHL, a national coordination approach has only been launched in 2024, pushed by the OECD recommendation as part of the OECD assessment of the Luxembourg public authorities’ response to COVID-19 (see section 2.5 and Box2.2). In the future, a new entity (National Purchasing and Logistics Centre) will mutualize purchasing and logistics activities in the health care sector (Luxembourg Government, 2023f).
Box2.2
The share of generics in the total pharmaceutical market in Luxembourg is the lowest in reporting OECD countries in 2021, with only 17.6% in volume (and 5.1% in value). For comparison, the rate for volume is 83.4% in Germany, 78.6% in the Netherlands, 66.9% in Denmark, 35.9% in Belgium and 29.3% in France. As described in section 5.6, substitution is authorized for two pharmacotherapeutic groups only (CSS Art. 22bis). The substitution of biosimilars is not authorized in Luxembourg. Unlike in other countries, Luxembourg has not implemented incentives for physicians and pharmacists to boost generic markets (OECD, 2023). The SHI funds a fixed reimbursement amount in the two authorized groups, allowing patients choice between the originator or a generic, but with responsibility for any price difference. In practice, the patient is not consistently presented with sufficient information to make an informed decision.
Task-sharing presents significant potential for enhancing efficiency and accessibility within the health care system (WHO/PEPFAR/UNAIDS, 2007). However, Luxembourg faces challenges in fully embracing this approach because of its regulations concerning health and care professionals. While multidisciplinary teams are prevalent in hospital settings, they remain largely absent in outpatient care, limiting the scope of task-sharing. Moreover, existing financing arrangements do not incentivize the establishment of multidisciplinary offices in outpatient settings, further impeding progress in this area. A legal framework is under development for medical practices, enabling doctors and health care professionals to form corporations (see section 6.2).
Luxembourg continues to use various information technology systems that lack interoperability, leading to non-standardized data recording in most cases. Although electronic versions of medical documents exist, they are predominantly used for internal purposes. As a result, the exchange of medical data in Luxembourg continues to heavily rely on traditional paper-based forms, resulting in a lack of efficiency.