-
10 January 2025 | Policy Analysis
Estonia implements compulsory liability insurance for healthcare providers -
20 November 2024 | Country Update
Estonia establishes legal framework for patient safety -
22 March 2024 | Country Update
Estonia’s new user-friendly Health Portal enhances access to health history
2.8. Person-centred care
As of 1 November 2024, Estonia has introduced a non-fault-based compulsory liability insurance system for healthcare providers, commonly known as patient insurance [1, 2]. The initiative aims to enhance patient safety, reduce preventable harm, and streamline the compensation for patients who experience avoidable health damage during medical care. All healthcare providers who are registered as a legal entity (for example, self-employed physicians, hospitals) were given a one-month transition period to comply with the new regulations, requiring them to secure liability insurance contracts by 1 December 2024. As of 19 January 2025, 94% of licensed health care providers (2,735 out of 2,915) have obtained the necessary insurance. Non-compliant providers risk having their operating licenses revoked by the Health Care Board [3].
The groundwork for this system began over a decade ago. The draft legislation was first submitted for public consultation in 2017, with both private and public models considered. Estonia ultimately chose a private model, citing its successful experience with mandatory motor vehicle insurance. This approach aimed to avoid the administrative complexity and costs of establishing a new public entity while benefiting from the flexibility of private insurers [1].
A key characteristic of the new system is a court-free compensation process that eliminates the need to prove fault. Patients who experience avoidable harm can file claims directly with the insurer of the healthcare provider, bypassing lengthy litigation process. Insurers must review claims within 180 days, with possible extensions if necessary. Compensation is capped at EUR 100,000 per patient per incident, with an annual limit of EUR 3 million per healthcare provider. Non-material damages, such as pain and suffering, are capped at EUR 30,000 per case. Patients who disagree with an insurer’s decision can appeal to an independent conciliation committee established under the Health Board. To further enhance patient safety, Estonia introduced a centralized database (POHAK) to systematically document patient safety incidents [4].
Drawing from the experience of similar systems in countries like Finland, the new scheme is projected to handle approximately 1,500–2,000 cases annually, with compensation granted in about 500 cases. For comparison, in 2023, the Estonian Healthcare Quality Expert Commission (EHQE), which patients turn to when dissatisfied with healthcare quality and unable to reach agreements with providers, reviewed 164 cases, identifying shortcomings in 38 instances, including 28 cases of medical errors. There is no public data on how many cases were resolved through direct compensation agreements between patients and healthcare providers without the commission’s involvement. The EHQE will cease operations in March 2025 when direct handling of claims with insurers becomes fully operational.
The financial impact on health care providers is expected to be minimal, as many already had voluntary insurance policies before the mandate. Premiums will vary based on provider type and the risk associated with their services, with an estimated budget increase of about 0.5%. The Ministry of Social Affairs anticipates that approximately half of these costs will be offset through higher service prices under contracts with the Estonian Health Insurance Fund (EHIF). To cover this, the EHIF received an additional EUR 2.2 million budget transfer for its 2025 budget, though the exact methodology for fund allocation is still in development [5].
However, the system faced an unexpected challenge: only one insurance company offered coverage, leading to concerns over high premiums. Healthcare providers pushed for a last-minute delay, arguing that the lack of competition had driven up costs. Despite these concerns, the government proceeded with the implementation as planned. The Ministry of Social Affairs has committed to analyzing the system’s performance after three years of implementation.
Authors
References
[1] Compulsory Liability Insurance of Healthcare Providers Act- Legislative Process https://www.riigiteataja.ee/eelnoud/menetluskaik/SOM/19-0548
[2] Compulsory Liability Insurance of Health Care Providers Act: https://www.riigiteataja.ee/en/eli/516092024001/consolide
[3] https://www.err.ee/1609538902/patsiendikindlustusega-pole-uhinenud-monisada-tervishoiuasutust
Authors
2.8.1. Patient information
The main place for personal health information is the Patient Portal (www. digilugu.ee – TEHIK, 2023), the output of the ENHIS introduced in 2008. The Patient Portal provides comprehensive information related to the use of health care services; it allows patients to fill in health declarations, apply for health certificates and book appointments (option available from 2019). The main aim of the portal is to make health information available to patients and health professionals, thereby improving the continuity and integration of care. Patients have the right to decide who can access their personal information. In addition, Estonian residents have access to personal information such as insurance coverage, benefits received, reimbursed costs of health care services and medicine use through the State Portal (www.eesti.ee – Riigiportaal, 2023), which as a patient portal uses digital authentication for privacy protection (see section 4.1.3 Information technology and e-health) (Table2.2). As part of the new-generation health information system project, the patient portal is being updated with a new user-friendly interface and new services. The updated patient portal will be called Terviseportaal and the first updated electronic services have been available since spring 2023. The renewal phase will be completed by the end of 2023.
Table2.2
Information related to health insurance, services, benefits and other entitlements is available from a variety of sources. The EHIF provides online reports on health services and benefits utilization, as well as lists of contracted health service providers and quality indicators. It also publishes information about entitlements on receiving cross-border care in the EU. More than half of Estonian citizens (59%) use the State Portal as their main source of information on work incapacity and health care benefits, followed by their family physician (29%) and the EHIF information line (19%) (Kantar EMOR, 2022).
The EHIF maintains a website (www.Ravijuhend.ee – Tartu University & EHIF, 2023) that compiles the national guidelines and related patient materials. The Health Board manages a vaccination information website (www.vaktsineeri.ee – EHIF, MoSA & Health Board, 2023) and Poison Information Centre Infoline website (www.16662.ee – Health Board, 2023). In addition, the NIHD manages a health information platform (www.terviseinfo.ee – NIHD, 2023b) and dedicated websites on alcohol, HIV, drug prevention and harm reduction, nutrition and tobacco. The sites include information resources on services as well as internet-based counselling services. During the last year, 11% of the Estonian population have visited these national portals (Kantar EMOR, 2022). The NIHD’s dedicated websites are in Estonian and Russian, and have become a valuable source of information for residents of other countries as well, with 78% of Internet traffic on www.alkoinfo.ee (NIHD, 2023a) coming from abroad, 72% on www.narko.ee (NIHD, 2023d) and 46% on www.hiv.ee (NIHD, 2023c) in 2022. Health service providers are legally obliged to provide information on the availability, accessibility and prices of services, which is mostly done through the websites.
Since 2012, the EHIF has been reporting selected quality indicators of hospitals in the Hospital Network Development Plan (HNDP). In 2016, it published the first report on quality indicators of selected medical specialties, including the information on the performance of family physicians under the umbrella of the family physician quality bonus system (QBS). The EHIF releases this information on an annual basis (Table2.2) (see sections 7.1.1 Transparency and 7.4 Health care quality).
In addition to the national authorities, in recent years more health care providers have made patient information (for example, patient guidelines, replies to complaints) accessible on their websites (Table2.2). The information is available in Estonian, selectively in Russian and increasingly in English, and recently also in Ukrainian to ensure access to relevant information for Ukrainian refugees who have arrived in Estonia.
To further promote a people-centred healthcare system, the Estonian Health Insurance Fund (EHIF) in cooperation with the Health and Welfare Information Systems Centre (TEHIK) recently launched a new Health Portal. This advanced platform, owned by the EHIF and TEHIK, replaces the previous patient portal that has been in operation for the past 15 years. The revamped portal not only features an improved user interface and usability, but also introduces the innovative “My Health History” feature. This feature allows users to easily search and filter past medical records, including appointments, test results, hospitalizations, and other interactions with healthcare providers.
Later in 2024, the portal will become even more comprehensive with the integration of a national e-booking system. This will transform the Health Portal into a one-stop digital hub for all health-related services, accessible to all residents of Estonia.
This step underscores Estonia’s commitment to fostering an environment where citizens can actively participate in health-related decision-making and feel more empowered in their health management.
The development of the Health Portal has been co-funded by the European Regional Development Fund with a total investment of €1.24 million.
Authors
References
https://www.terviseportaal.ee/en – access to Health Portal
https://www.terviseportaal.ee/en/uudised-ja-uuringud/uudised/0 (in English)
https://www.tervisekassa.ee/uudised/uus-terviseportaal-vahetas-valja-senise-digiloo – (in Estonian)
2.8.2. Patient choice
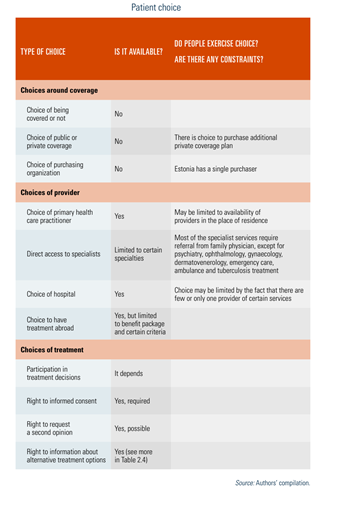
The EHIF provides almost universal coverage and its range of benefits is broad (see section 3.3.1 Coverage). As Estonia has a single-payer system, there is no competition or choice between different purchasing organizations. Since 2006, patients have been able to choose their health care provider from among the EHIF’s contractual partners. Before that, the choice was limited to the contracted providers of the EHIF regional department where a given patient was registered (Table2.3). At the PHC level, all Estonian citizens should register on a patient list with a family physician of their choice. Family physicians may refuse an individual if the list is full or if the person does not live in their catchment area (see section 5.3 Primary care). A referral also gives the patient a free choice of specialist or a provider, such as a hospital, which only 65% of the population are aware of (Kantar EMOR, 2022). However, this freedom of choice may be constrained by waiting lists or proximity to the provider. Providers without a contract with the EHIF are freely accessible to anyone willing to pay out of pocket.
Table2.3
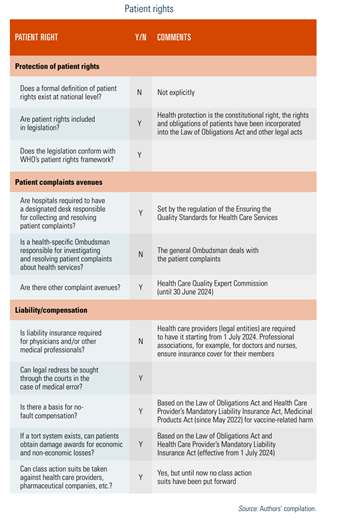
2.8.3. Patient rights
Although there is neither a definition nor a single law on patients’ rights, the principles of the Declaration on the Promotion of Patients’ Rights in Europe (WHO Regional Office for Europe, 1994) have been incorporated into several legal acts (Table2.4). First of all, the Estonian Constitution states that “everyone has the right to the protection of health”. The Law of Obligations Act defines the contractual relationship between the patient and the doctor, and requires the involvement of patients in decisions regarding their own health. Health care providers need a signed, written informed consent before providing health services to patients. Doctors must inform patients about their concerns and the required services. The Act also states that a provider cannot promise the success of an operation or a recovery. According to the Health Insurance Act, patients have the right to a second opinion, and the Health Services Provision Act ensures that everyone has access to emergency care. The Personal Data Protection Act covers the provisions to ensure the confidentiality of personal health information.
Table2.4
Quality standards for health care services and the conditions of health care facilities are regulated by different legislative acts. Although standards are specified and include requirements for easy accessibility for all, in reality many older facilities do not fully meet the mobility needs of disabled people.
The Health Services Organization Act and the Law of Obligations Act jointly regulate the complaint procedures for health services and make the health care provider responsible for malpractice and low quality of health services. Most complaints are settled directly between the health care provider and the patient, and there are no official data on how often this occurs. The patient has the right to have the case heard in court and the Health Board can impose a fine or withdraw the licence of the health care provider concerned. For dissatisfaction of health service quality, a patient can also turn to the Health Board, which can initiate an inspection. If a patient’s health is suspected to have been harmed or if there are serious quality problems, official complaints are lodged with the Health Care Quality Expert Commission, which acts under the MoSA. The judgements of the Commission can be used to support the court appeal. This approach will be effective until 1 July 2024, when the new Health Care Provider’s Mandatory Liability Insurance Act, which was passed in April 2022, will come into force. This act requires all health care providers to have liability insurance. The Health Care Quality Expert Commission will also cease to exist and be replaced by the Liability Insurance Reconciliation Commission.
In 2021, the Health Care Quality Expert Commission managed 168 patient complaints (Table2.5); 42 (25%) were related to malpractice, of which 32 (66%) were related to medical errors. Since 2005, the total number of complaints has increased considerably, particularly since 2016. A substantial rise in the number of complaints could indicate a rising awareness about this tool among the population in Estonia. The Health Care Quality Expert commission is the only expert on patients’ rights in Estonia.
Table2.5
Another mechanism for patient participation, in addition to representation on the EHIF Supervisory Board, is the patient advisory committees. These committees were established in 2019 at some hospitals, starting with Kuressaare Hospital and Tartu University Hospital and followed by others. The purpose of the patient advisory committees is to advise the hospital management board on the development of health care services, and to help bring the perspective of patients and their caregivers to the fore. The committees work on a voluntary basis.
Since 1996, the EHIF has conducted annual surveys on patient satisfaction with various aspects of the health system. The scope of the surveys has been broadened over time and now also allows for longitudinal observations. In general, population satisfaction with access to health services and their quality has been relatively high over the years.
2.8.4. Patients and cross-border health care
Insured individuals are entitled to receive services covered by the EHIF in the other EU Member States, Iceland, Liechtenstein, Norway and Switzerland. Directive 2011/24/EU on patients’ rights in cross-border health care sets out the conditions under which a patient may travel on their own initiative to another EU country to receive medical care and be reimbursed. Furthermore, based on European Commission Regulation 883/2004, insured Estonians can use the European Health Insurance Card to receive health services abroad under equal conditions and tariffs as nationals of the Member State. Treatment is paid for by the EHIF during a temporary stay. Travel costs are not covered.
In addition, every insured person can apply to the EHIF for pre-authorization when treatment is not available in Estonia or when the patient is planning treatment abroad. Treatment cannot be denied if it is included in the Estonian basic benefit package and cannot be provided in Estonia within a medically justifiable time limit. EHIF payments for health care abroad have increased from €1.4 million in 2008 to €5.8 million in 2020 and dropping to €3.0 million in 2021, possibly as a result of the COVID-19 restrictions (EHIF, 2021b). Information on the authorizations granted by the EHIF is available and published in the annual reports. In 2021, 31 persons were referred for treatment abroad, eight for examinations, and 38 for unrelated bone marrow donor search through the Finnish Red Cross. In the last five years, more than two thirds of cross-border health care was provided in Finland, Latvia, Germany and Spain (EHIF, 2017, 2018, 2019, 2020a, 2021b).
Cross-border health care is supported by an innovative and forward-looking exchange of health data with Finland, Croatia, Portugal, Poland and Spain, enabling the use of cross-border digital prescriptions in these countries. This is the result of an EU-wide initiative launched in 2017 to expand the cross-border data exchange and digital prescribing to other EU countries.