-
20 May 2025 | Country Update
The National Plan for the Development of Geriatric Care in Czechia until 2035 -
25 July 2024 | Country Update
Delegated prescription for oncological patients – from complex centres to regions -
01 March 2024 | Country Update
Strategic planning of care for the ageing population
5.4. Specialized care
Czechia’s National Plan for the Development of Geriatric Care until 2035 responds to ongoing population ageing. The plan outlines four main strategic goals:
- Creating conditions for healthy ageing and the prevention of disability,
- Ensuring high-quality geriatric care supported by research and education in geriatrics and gerontology,
- Improving the accessibility and systemic organization of specialized geriatric care, and
- Establishing effective integration within the geriatric care system to meet the complex needs of older patients.
The accessibility of specialized geriatric care is to be ensured through four major areas:
- a network of geriatric clinics at all medical faculties,
- the establishment of a basic network of inpatient geriatric care facilities,
- geriatric outpatient clinics, and
- systemic support to guarantee the availability of geriatric health services.
With proper diagnosis and appropriately tailored treatment, patients with frailty, multimorbidity, and sarcopenia can spend more time at home and in community environments to treat conditions appropriately and in a timely manner. This shift can contribute to greater long-term fiscal sustainability and enhance the role of community- and family-based care, while simultaneously supporting the fullest possible return to quality of life and self-sufficiency through adequate follow-up care and rehabilitation. On the other hand, hospitalization in a dedicated geriatric ward has the potential to improve patients’ functional outcomes at discharge, increase the share of patients returning to their home environment, reduce the number discharged to subsequent inpatient facilities, and lower the rate of early rehospitalizations.
The plan furthermore includes detailed sub-goals and is supported by an analytical study conducted by the Institute of Health Information and Statistics (ÚZIS).
Authors
Authors
On 24 January 2024, the Ministry of Health in Czechia launched a project to support the planning of the development of integrated health and social care. This three-year project is aimed at reacting to the rising needs of the gradually ageing population and growing number of chronically ill patients. The goal is to map the existing health and social services around Czechia and identify what is missing. The ambition is to determine specific steps to fill these “white spaces” (bílá místa). A preliminary investigation shows that one of the problems might be the lack of rules and conditions for the cooperation and coordination.
Methodological guidelines for the creation of regional health and social plans should be created in cooperation with the Ministry of Labour and Social Affairs and other partners of the project: the representatives of regional administration, health insurance funds, representatives of health and social service providers, and representatives of the clients/patients. The project will take place in all 14 regions and will also include training of officials of the health and social departments of individual regional offices.
Authors
5.4.1. Specialized ambulatory care (outpatient)
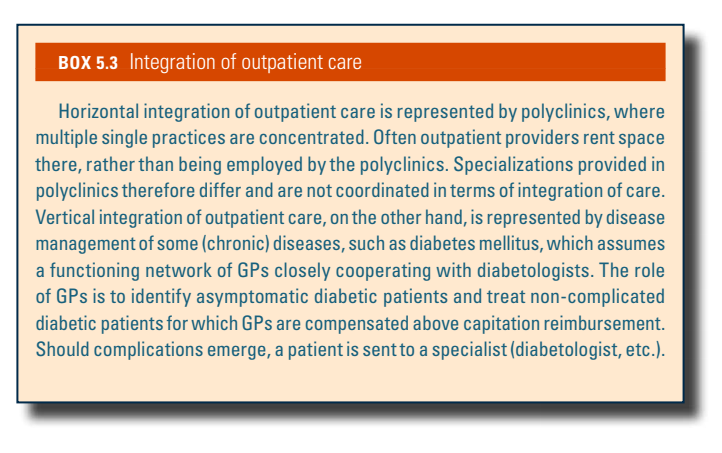
Similar to primary outpatient care, specialized outpatient services in Czechia are offered by self-employed specialists in solo or group practices, health centres or polyclinics (see Box5.3), or employed in hospital outpatient departments. As stated above, patients generally have the possibility to visit specialists without referrals and frequently do so.
Box5.3
Outpatient specialists cover 56 specializations and include non-physician specializations such as clinical psychologists, clinical speech therapists, eyesight therapists, orthoptists and audiologists. The distribution of outpatient specialists is uneven across the country, particularly for some specializations (see Box4.2; density maps for each specialization are also downloadable from VZP’s website: https://www.vzp.cz/poskytovatele/dostupnost-zdravotni-pece/ambulantni-pece). Prague (with 64.2 physicians per 100 000 population in 2019; national average 37.3 per 100 000) is densely populated by all outpatient care specializations, while border areas are generally less dense (ÚZIS, 2020a). Minimum legislative limits as set by Governmental Regulation no. 307/2012 Coll. (2012) must be met across the country, however, meaning certain specializations must be accessible within 45, 60, 90 or 120 minutes. HIFs must contract outpatient care specialists to guarantee these limits for their members.
Box4.2

5.4.2. Day care
Day care is defined as the provision of a bed for a patient for less than 24 hours (Health Service Act, 2011). The exact time of care provision depends on the clinical examination or surgery. Besides hospitals providing inpatient care, day care may also be offered by facilities without inpatient departments if conditions to run a health care facility (hygienic, technical and personnel) and to perform the specific procedure are fulfilled. One of the conditions for day care provision is that a standard inpatient care facility must be accessible within a reasonable distance for follow-up in case of complications.
Day care is provided for six specializations: surgery (including ocular, paediatric and vascular), cosmetic surgery (including burns), gynaecology, urology, orthopaedics and otolaryngology (including jaw surgery). Procedures carried out in emergency departments cannot be classified as day care under any circumstances. If carried out in other than surgical specializations above, the procedures must be invasive. Day care is only for patients with minimal medical risk. If a patient suffers from comorbidities or has health risks, inpatient hospitalization is provided, though day care provision is still possible.
Except for ocular surgeries (90% of day care) and partly orthopaedics, day care is underdeveloped in Czechia compared with many EU countries (Advanced Healthcare Management Consulting, 2022). The share of day care reaches 5–10% of all interventions suitable for day care, whereas other countries reach 50% and target even 75%. Advanced Healthcare Management Consulting (2022) show savings of 300 000 inpatient days in their model for 23 day care interventions (out of 200 interventions that could be carried out as day care); so as much as 20% more surgeries could be carried out compared with the current situation if care was better organized. This, however, would also require a strong system for follow-up care and support systems at home after discharge, without which day surgeries are not feasible. In 2019, day care was provided on 246 beds in Czechia. A total of 43 providers offered exclusively day care services at 69 different sites (ÚZIS, 2020a). Some providers provided day care alongside acute inpatient care, the data for which are not statistically collected. On the other hand, some outpatient providers categorized more difficult interventions as day care, which overestimates numbers (Advanced Healthcare Management Consulting, 2022). Eye surgeries, the most common day care treatment in Czechia, are also neither separately categorized in Czech data nor in European data (Eurostat, 2022).
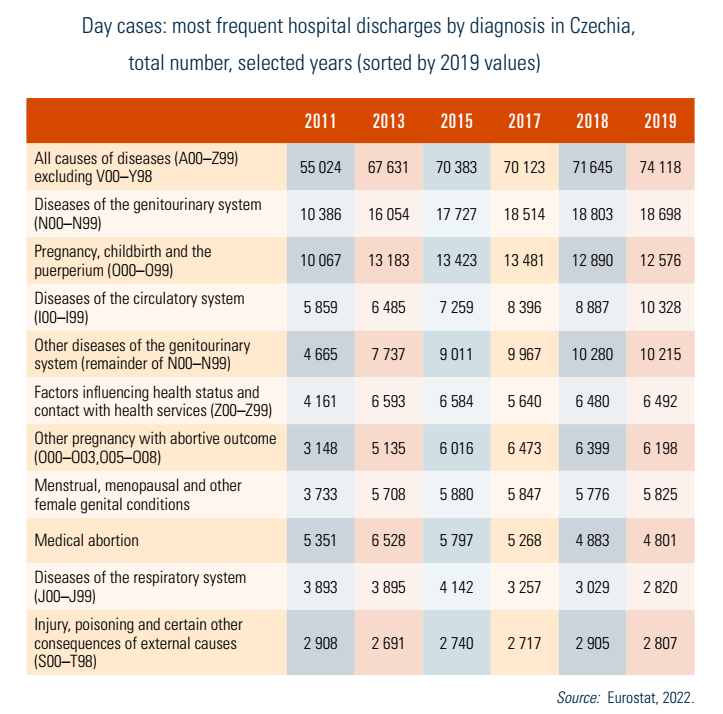
Table5.1 shows the total number of cases and most frequent diagnoses treated as day cases per Eurostat categories of day care; the number of day cases (all causes) has risen by 50% since 2011 in Eurostat definitions. All selected causes saw an increase, except for medical abortions, respiratory diseases and injuries. The decrease of medical abortions as day cases stems from the general downward trend of medical abortions in Czechia (ÚZIS, 2020b). Note that medical abortions nearly doubled between 2002 and 2011 (Alexa et al., 2015). Gynaecological and genitourinary conditions were mainly treated as day cases in 2019.
Table5.1
5.4.3. Inpatient care
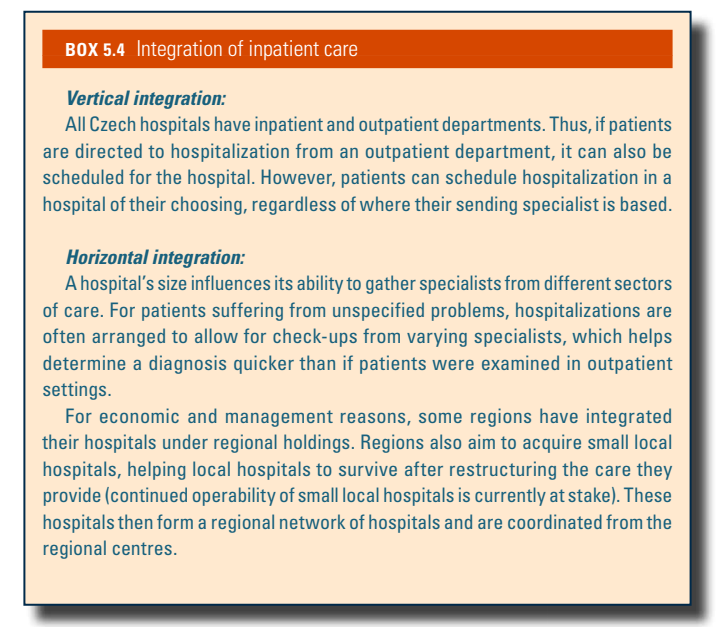
Inpatient care in Czechia is provided in hospitals and specialized inpatient facilities (see Box5.4). As described in section 5.2, access to specialist care is not restricted by gatekeeping, though referrals are necessary for hospitalization (except in cases of medical emergency, including life-threatening situations, childbirth or law-mandated hospitalization, such as highly contagious individuals). In case of emergency, patients are unlikely to be able to choose a hospital, except in most cases of childbirth, though pregnant women in most regions need to register in advance with the hospital of their choice for capacity reasons.
Box5.4
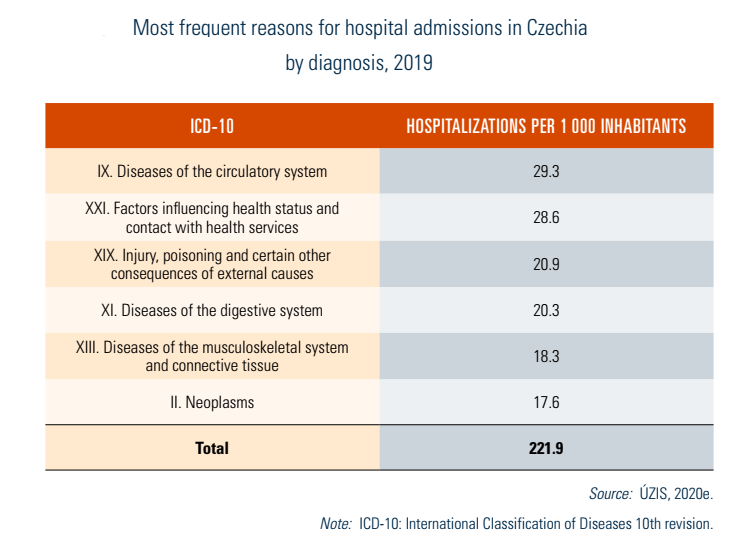
A referral must contain the physician’s written justification for hospitalization and any other important information about the patient’s health status. Patients can usually go to a hospital of their choice if that hospital has a contract with their HIF. The most frequent reasons for hospitalizations are listed in Table5.2.
Table5.2
There were 194 hospitals in Czechia providing 60 500 beds in 2019; 40 hospitals provided LTC only, covering 3078 beds. Acute care hospitals usually also provide some LTC beds in addition to acute care beds, summing up to approximately 16% of hospital beds. There were also 119 specialized therapeutic institutes with 16 937 beds, 52% of which were devoted to psychiatric care (both for children and adults). There are regional disparities in hospital densities (see section 4.1).
Large hospitals providing maximum care are situated exclusively in larger cities. Hospitals in smaller cities and towns tend to focus on a limited number of medical specialties (for example, internal medicine and maternity wards) and the scope of care offered is less broad. In recent years, some of these hospitals have focused on day surgery and reduced their inpatient services to focus more on outpatient services.
Teaching hospitals, which are directly subordinated to MZČR (except for one that is subordinate to the Ministry of Defence), have a special status, as they perform educational and research duties in addition to their function as providers. MŠMT oversees instruction carried out in teaching hospitals (see section 4.2), which tend to have high-end technologies, which is also in line with their teaching mission.
Section 112 of the Health Service Act (2011) defines conditions for the set-up of centres of highly specialized care (CHSCs). CHSC applications must be approved by MZČR, after which they can obtain a special reimbursement contract based on the costly care and pharmaceuticals provided; only CHSCs can prescribe type S pharmaceuticals (exceptionally costly pharmaceuticals). They also provide care using costly equipment reimbursed from SHI. A list of CHSCs in different specializations is provided on MZČR’s website (at https://www.mzcr.cz/category/agendy-ministerstva/zdravotni-sluzby-agendy-ministerstva/centra-vysoce-specializovane-pece/seznam-center-vysoce-specializovane-pece-v-cr/page/2/).
Long-term care and nursing care in Czechia involve the health and social care systems, not being a separate branch of either (see section 5.8); informal care may also substitute for portions of institutionalized LTC (see section 5.9). Although the number of LTC beds has recently risen (be it in health or social care), patients sometimes tend to stay longer than necessary in acute care beds instead of being transferred to LTC, raising hospitalization costs.
