-
25 March 2025 | Country Update
New agreement on faster diagnosis for people with dementia
5.4. Specialized care
5.4.1. Specialized ambulatory care
Specialized ambulatory care is mostly provided in hospitals. According to WHO data, ambulatory visits are lower in Denmark than the EU average. Ambulatory activity has increased substantially over the past 20 years due to initiatives to increase efficiency in the health system. The average length of hospital stay is now shorter than in past decades, and more diagnostics and treatment occur in outpatient clinics.
Patients also have free access to the full range of private specialists practising outside hospitals upon referral from a GP. Specialist doctors work on a private basis and are reimbursed by the regions. They must have a provider number from the region to receive reimbursement. Privately practising specialists can refer patients to public hospitals.
With the health care reform of 2022 (see Chapter 6), it was agreed that up to 25 “local hospitals” will be established in areas that, in a Danish context, are far from the nearest hospital. Up to DKK 4 billion (€536.4 million) was allocated to set up the 25 “local hospitals” but not for their ongoing operation. The “local hospitals” are planned to be for specialized outpatient procedures, including uncomplicated diagnostic examinations such as X-rays, blood tests or ECG and outpatient follow-up, but they will not have beds. The implementation of the decision is awaiting a broader health system reform initiative which is expected in 2024.
5.4.2. Day care (hospital ambulatory care)
Day care takes place at hospitals and includes the medical and paramedical services delivered to patients formally admitted for diagnosis, treatment or other types of health care performed without overnight stays. The most common day care is same-day surgery; a special category within day care is births. Women who have given birth before and deliver with no complications are often discharged on the same day. There are exceptions, and most women giving birth for the first time are discharged after the first night. In 2018, 30% went home within 12 hours of giving birth, and just over half (56%) were home within two days, while 17% were hospitalized more than three days after birth (Sundhedsstyrelsen, 2022b).In 2024, around 40,000 Danes aged 65+ were officially diagnosed with dementia, but estimates suggest the actual number was closer to 97,000. By 2035, approximately 134,000 Danes are expected to live with dementia [1].
To improve timely dementia diagnosis and ensure faster access to treatment, the government and the interest organization for the regions, Danish Regions, have allocated DKK 35 million (around EUR 4.7 million) in 2025 and 2026. The funds will be used to increase the capacity of regional diagnostic units and also support additional initiatives based on upcoming recommendations from the Danish Health Authority on strengthening dementia diagnostics. This could include, for example, increasing the number of diagnostic procedures outside hospitals [1].
Authors
5.4.3. Inpatient care
Most secondary and tertiary care takes place in public hospitals owned and operated by the regions. Doctors and other health professionals are salaried hospital employees. Hospitals have inpatient and outpatient clinics, and some also have 24-hour emergency wards. Outpatient clinics are often used for pre- or post-hospitalization diagnosis and treatments. Most public hospitals are general hospitals with different specialization levels. There is no official classification of hospitals according to the level of specialization, technological equipment or performance, but hospital functions (departments) within hospitals are classified according to level of specialization which is subject to approval by national-level authorities according to the specialty planning process. Since Denmark is a small country with good transportation infrastructure, the concentration of highly specialized services in just a few hospitals does not present a major barrier to access.
Contracting with private hospitals is limited by the regions and used mainly for specific interventions, such as bariatric surgery, or when the regions cannot uphold the waiting time guarantees (see section 5.2). Out of the region’s total operating costs, the share spent on private providers of hospital services is relatively small, although it appears to be increasing. In 2020, approximately 120 000 patients were investigated and treated at private hospitals at public expense. The cost of this amounted to DKK 706 million (€94.7 million) (Danske Regioner, 2021b).
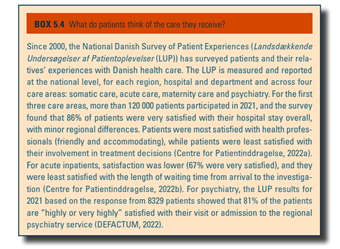
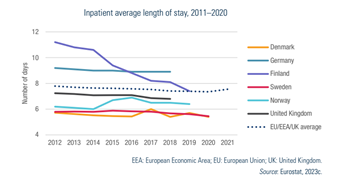
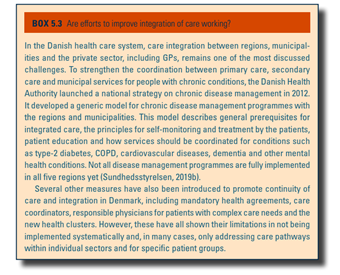
Since the 1940s, there has been a focus on reducing the length of stay in hospitals (Fig5.2). If the municipality cannot provide the necessary home nurse services or bed space in, for example, a nursing home after hospital treatment, the municipality pays a daily rate to the region and the state. Until recently (see section 7.2.3), there was a general movement to establish larger and more specialized units of hospitals, followed by closing smaller entities to strengthen the quality of care. Similarly, the regions have built or are currently building several new, modern hospitals that are considered future-proof with the goals of ensuring better and more cohesive patient treatment, improved patient safety, greater efficiency and higher quality (see sections 6.1 and 7.4). The construction projects are funded by the state-financed Kvalitetsfonden and the regions (Danske Regioner, 2021a). Efforts are being made to improve cooperation between GPs and hospitals by appointing coordinators to work closely with hospital departments and report back to the GPs. Likewise, new health clusters aim to create better continuity of care (Box5.3). Free choice of hospital after a referral has also encouraged hospitals to improve information to GPs about discharges and services in general. Overall, satisfaction with the health system is high (Box5.4).
| Fig5.2 | Box5.3 |
 |  |
Box5.4