-
11 May 2025 | Country Update
Health Insurance Fund reserve for 2024
3.3. Overview of the statutory financing system
The financing of the GeSY is tripartite, based on health contributions from beneficiaries, employers and the state. A very low percentage of funding comes from co-payments, as well as EU grants. Contributions are compulsory for all beneficiaries if they have a declared annual income.The surplus of the Health Insurance Fund for 2024 amounts to EUR 113 million, with the fund’s accumulated reserve totalling EUR 707 million, which corresponds to approximately 4.6 months of payments.
Specifically, based on the unaudited financial statements, the fund’s total revenue for 2024 amounted to EUR 1,839 million and total expenditure to EUR 1,726 million, with net surplus for the year totalling EUR 113 million.
The fund’s positive financial position enables the Health Insurance Organisation to further expand and improve the services offered, introduce new technologies and embark on new projects, such as the programme to manage patient missions abroad for certain treatments not available in Cyprus under the general healthcare system (GeSY), which is expected to start on 1 October 2025.
The fund’s reserve is estimated to remain at approximately the same level at the end of 2025, which also depends on the development of the economy, on which the fund’s income mainly depends.
References
3.3.1. Coverage
BREADTH: WHO IS COVERED?
Coverage is universal and entitlement is based on legal residence, being no longer linked to citizenship, income or payment of contributions. Thus, the vast majority of the population is covered, including EU and non-EU citizens, refugees and people with subsidiary or international protection, as well as their families and dependants (GeSY, 2024a). Unemployed persons and recipients of the Guaranteed Minimum Income (GMI) benefit[2] or public assistance (including disability) are also covered free of formal contributions, provided their status is certified by the Welfare Benefits Administration Service (WBAS) and the Social Welfare Services (SWS) of the MLSI. The family and dependants of beneficiaries are also covered without obligation to pay formal contributions. There are no potential beneficiaries of the new system who opt for alternative forms of coverage. What every beneficiary needs to do to be able to visit any system’s provider is to register and open an account at the GeSY beneficiary portal (GeSY, 2024a).
Asylum seekers are not covered by the GeSY. Instead, they are entitled to free care from the SHSO and have access to all public hospitals and health centres. More specifically, they are entitled to free medical care, which includes emergency medical services and basic treatment of diseases in public medical institutions. The MoH grants free access to all asylum seekers, regardless of whether they are supported by the SWS, provided they apply to confirm their residence status and then receive their medical card, which is valid for one year.
Undocumented migrants and non-EU students are not covered by the GeSY. The first category includes all asylum seekers whose applications have been rejected, migrants whose visas and work permits have expired and who have nevertheless remained in Cyprus without official documents, and other undocumented migrants. Nevertheless, it is common practice that they are accepted for examination and basic treatment in the A & E departments of public hospitals. There have also been a few cases where the HIO, exercising its statutory discretion, has authorized the care of undocumented migrants on the basis of an urgent and life-threatening medical need.
Students from non-EU countries who wish to study in Cyprus are required by law to pay for VHI from their own funds. Such insurance is a prerequisite for the necessary registration with the Civil Registry and Migration Department. This private annual insurance allows them to use private or, in some cases, public sector health care services, for which a fee is charged, which is then reimbursed by the insurance company.
SCOPE OF COVERAGE
The benefit package of the new health care system is quite comprehensive and uniform for the entire insured population. The benefits provided are explicitly set out in national legislation (Law 74(I)/2017), and in regulations and guidelines issued by the HIO from time to time as required. All services are provided by health care professionals contracted with the HIO, while the beneficiaries are free to choose their providers in accordance with the provisions of the above law.
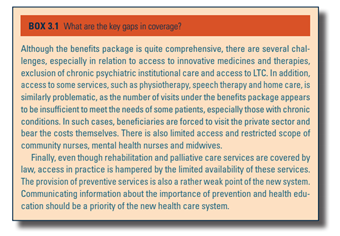
Health services covered under the GeSY include care by personal and specialist doctors, laboratory tests and diagnostic examinations, and necessary medicines, medical devices and medical supplies provided on medical or dental prescription, which must be included in the positive list of reimbursable medicinal products or the positive list of medical devices and medical supplies. Under the conditions set out in the HIO’s internal regulations, the administration of medicines, medical devices and medical supplies not included in the two lists above may be permitted in some cases. The package of services also includes health care services provided by nurses and midwives, and care by other health professionals (who are not doctors); palliative care; inpatient health care; limited preventive dental care; medical rehabilitation, including the supply, maintenance and renewal of orthopaedic and orthotic items and prostheses; home care; and emergency care (including ambulance services). The package of services does not include chronic psychiatric institutional or compulsory care provided under the provisions of the “Law on Psychiatric Care of 1997”, substance abuse rehabilitation services or mental health rehabilitation services such as day care centres (Law 77(I)/1997).
The contents of the two positive lists (the list of medicinal products and the list of medical devices and medical supplies) are defined and regularly reviewed by the HIO as new items and products are added or removed.[3] Over the period 2021–2022, key patient organizations, namely the OSAK and the Cyprus Alliance for Rare Diseases, have consistently reported that a large gap exists in access to new and innovative medicines under the GeSY, mainly due to deficiencies in HTA procedures (see also Section 2.7.3).
Even though the GeSY Founding Law clearly mentions all the services covered, in practice the timely access to some services such as palliative or rehabilitation services is not easy due to the small number of contracted providers, which in some cases leads to the creation of waiting lists.
Under the GeSY, almost all costs of statutory benefits are covered by the HIF. This, combined with low co-payments and annual caps, aims to ensure a high level of financial protection without any serious financial barriers to access. Problems with the financial burden on beneficiaries may arise in cases where there are gaps in coverage and difficulties in access and availability of services, as described in Box3.1.
Box3.1
- 2. The Guaranteed Minimum Income aims to ensure a minimum socially acceptable standard of living for individuals and their families legally residing in the Republic of Cyprus, as long as they meet the necessary conditions. In particular, any person whose income and other financial resources are not sufficient to cover their basic and special needs, as defined by the relevant legislation, may request the granting of the minimum guaranteed income, which is provided in the form of financial support and/or services. The allowance varies according to the applicant’s income. When the applicant’s income increases, the allowance decreases. The total amount the applicant receives varies depending on the members of their family and their special needs. See: https://www.wbas.dmsw.gov.cy/dmsw/ydep.nsf/grands01_el/grands01_el?OpenDocument ↰
- 3. For information on the lists of medicines within GeSY, see gesy.org.cy. ↰
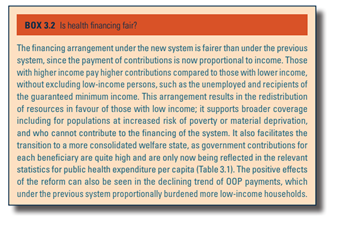
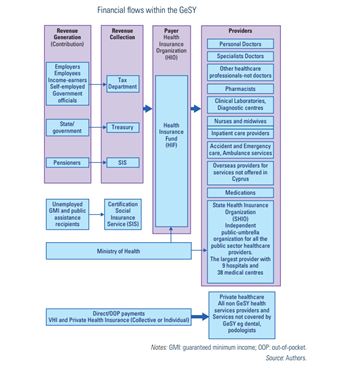
3.3.2. Collection
Since 1 July 2020, when the new health care system was fully implemented, income-based contributions are set as follows: i) employees, pensioners, government officials and income-earners, 2.65% of their gross income; ii) employer for each employee, 2.90% on their gross income; iii) self-employed 4.00%; and iv) state/government contributing 4.7% for each employee, self-employed person, government official and pensioner. The maximum annual amount of gross income on which contributions are paid is €180 000 (GeSY, 2024b).
Employers are required by law to deduct contributions from their employees’ salaries. The SIS is responsible for collecting contributions from employees, employers and the self-employed based on insurable income in accordance with the “Law on Social Insurance”. For the self-employed, contributions in excess of insurable income are collected by the Tax Department. The state’s contribution is paid by the Treasury. Finally, pensioners’ contributions are deducted from pensions and collected by the SIS and the Treasury. The contributions are then transferred to the HIF by these three designated authorities. The HIF is administered exclusively by the HIO, which is also the sole contracting and purchasing authority for GeSY services.
Contribution rates are prescribed by law and must be approved by the House of Representatives. Setting them was part of the creation of the GeSY legislation and the outcome of a continuous dialogue between all social partners and the state (see also Box3.2).
Box3.2
3.3.3. Pooling and allocation of funds
ALLOCATION FROM COLLECTION AGENCIES TO POOLING AGENCIES
Pooling takes place after the collection and transfer of all revenues from contributions into the HIF managed by the HIO (see Fig3.6 and Section 3.3.2). This means that the allocation of pooled funds is done by the HIO, which is the sole purchaser of services. Risk pooling serves the fundamental principles of “the healthy subsidising the sick and the young subsidising the old” and meets the objectives of financial protection and equitable access based on need.
Fig3.6
ALLOCATING RESOURCES TO PURCHASERS
Within the GeSY, the pooling and purchasing functions are integrated under the umbrella of the HIO. The fact that the HIO also acts as the single purchaser reduces the fragmentation of pooling and purchasing, and helps to keep the associated administrative costs lower. According to the law, the administrative costs of the HIO must not exceed 5% of its annual budget.
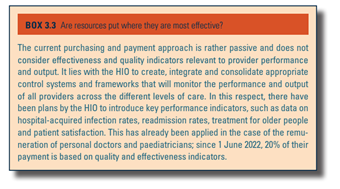
In addition, there is more room for effective monitoring of providers regarding abuses of the system (see Section 7.6.2). Institutionally, the power lies with the single purchaser and not with the providers. However, financial resources do not seem to be directed in a way that explicitly promotes efficiency and quality. The HIO has begun to consider these issues, but so far the measures taken have been limited (Box3.3).
Box3.3
The single-purchaser and single-payer system of the GeSY uses a payment method with a balanced incentive structure that allows providers to compete for patients based on quality, not price. Payment uses a mix of mechanisms for different levels of care. At primary care level, personal doctors are remunerated per capita, based on the number of patients registered on their list, while at the secondary level, hospitals and contracted specialties of the private sector are paid based on activity, within a framework of hard global budgeting (see Section 3.7). Nevertheless, the system is still far from adopting a strategic purchasing and payment approach, which would require indicators for needs assessment, capacity planning and quality of service provision to be included in the process of allocating pooled funds.
3.3.4. Purchasing and purchaser–provider relations
The organizational relationship between providers and the HIO is formalized through a contract. For public sector providers, the contract is between the HIO and the SHSO, on behalf of providers. For the private sector, a contract is signed between the HIO and each provider, which can be either a doctor, a hospital, a polyclinic or any other provider. In the first case, the communication is between the purchaser and the SHSO, and in the second, between the purchaser and the provider, if required. A common subject of a communication relates to the claims of private providers (unjustified claims, suspicion of supplier-induced demand, etc.). For issues related to changes in the nature of remuneration (for example, incentives and indicators of efficiency and quality, the introduction of protocols and guidelines, the operation of afternoon surgeries and university clinics in public hospitals, etc.), communication is with the medical associations (PIS, Association of Government Doctors (PASIKY) and Association of Private Doctors Contracted with the GeSY). At present, there is limited monitoring and enforcement of the contract, with only claims currently being sample checked.
In the first four years of operation of the GeSY, there is still a lack of specific mechanisms and monitoring frameworks that create incentives to improve quality and make efficiency gains. According to the Auditor General, “the introduction of effective retrospective audit procedures to monitor the quality and appropriateness of care is urgently needed” (Audit Office of the Republic of Cyprus, 2022a).