-
17 September 2025 | Country Update
Development of an integrated Early Childhood Intervention system -
21 July 2025 | Policy Analysis
A system of mobile health clinics is being launched -
03 September 2023 | Country Update
Reducing the administrative burden on primary healthcare doctors -
31 May 2023 | Policy Analysis
Report of the State Audit Office on the effectiveness of primary health care -
23 April 2023 | Country Update
Pilot project on preventive health examinations in five counties -
24 November 2022 | Country Update
Improving access to primary healthcare for third-country workers
5.3. Primary care
Primary care services are provided by a network of first-contact doctors and nurses contracted by the CHIF. Every insured citizen is required to register with a family physician (in the case of adults) or a paediatrician (in the case of preschool children), whom they can choose freely. Primary care physicians can be changed at any time free of charge. They serve as gatekeepers to secondary and tertiary levels of care. Upon referral, patients are free to go to a hospital of their choice.
Following an EU recommendation, a project aimed at ensuring that all family medicine doctors have a specialization in family medicine was started in 2003, with the overall goal of improving the quality of primary care. All practising primary care physicians were required to specialize in family medicine by 2015.
In 2018, out of a total of 2594 medical teams, 1408 were specialists in diverse fields (1033 in family medicine, 283 in paediatrics, 34 in occupational medicine, 40 in school medicine and 18 in other specialisms) (Croatian Institute of Public Health, 2019).
In Croatia primary care comprises the following services:
- general practice/family medicine;
- health care for preschool children;
- public health;
- women’s health care;
- nursing care at home;
- community nurse services;
- dental care;
- dental laboratory services;
- hygienic–epidemiological services;
- preventive–educational measures for health care of schoolchildren and students;
- laboratory diagnostics;
- pharmaceutical care;
- urgent medical care;
- palliative care;
- occupational health/sports medicine;
- mental health care, outpatient treatment of mental illness and disorders, including addiction;
- speech therapy;
- midwifery care;
- physical therapy;
- occupational therapy;
- ambulance transport;
- diagnostics in radiology;
- telemedicine;
- environmental health; and
- sanitary engineering.
Primary care services are provided in solo practices, larger units comprising several offices, and county health centres that provide general medical consultations, primary care gynaecology services, care for preschool children, dental care and community nursing care. Community nursing services comprise various preventive interventions provided in home settings and focus on patients with chronic conditions, pregnant women and mothers with infants. They are organized by the health centres and are delivered through nurses in cooperation with family physicians.
The number of group practices and interdisciplinary teams in primary care has been growing in recent years, specifically since 2013 when the CHIF started providing financial incentives to all family physicians who choose to open a group practice. Physicians working in concessions had advocated for more independence in business and decision-making, which has led to changes in the Health Care Act. From the beginning of 2019 there is a national upper limit of 25% of physicians and nurses in primary care (i.e. general practice, paediatrics and gynaecology) who can be employed by publicly run health centres. At least 75% work independently in group or, mostly, solo practices.
Each family physician contracted by the CHIF is expected to have at least 1275 registered patients on their roster and the maximum number of patients on a list is 2125. The number of 1700 patients is the commonly used standard, and is important for defining categories in the revenue model. Services are provided by teams consisting of a family physician and a nurse. Primary care for infants and preschool children is delivered by teams consisting of a paediatrician and a nurse, each with an average of 1200 patients on their roster. They provide preventive care (vaccinations) and general paediatric care. Children are registered with a paediatrician until the age of 7, when they are taken over by a family physician. Primary care gynaecology services include health maintenance examinations and treatment of disorders of the female reproductive system, as well as maternity care. The prescribed standard number of patients per primary gynaecological team (a gynaecologist and a nurse) is 6000 women.
In many areas of the country, there are difficulties in organizing continuous provision of primary care and finding replacements for health workers during annual or sick leave. Moreover, often there is no appropriate communication between family medicine doctors and the community, pharmacists and other health workers. Due to long waiting times, patients often skip primary care to access specialists directly, mainly through emergency departments. Patients tend to have low trust in primary care physicians and rely more on hospital specialists, diagnostics and treatment. A major challenge is that primary, secondary and tertiary care function largely independently from one another, lacking integration and communication.
Formally, patients cannot access specialists directly (if services are to be paid by mandatory health insurance), unless they have previously consulted a primary care physician or need emergency care. In 2018 there were 38.2 million visits to family medicine offices, of which 12.6 million were with family physicians and 25.6 million with other health professionals (Croatian Institute of Public Health, 2019).
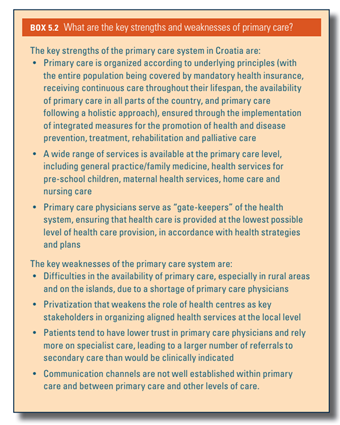
Box5.2 describes key strengths and weaknesses of the primary care in Croatia.
Box5.2
The development of a sustainable, integrated Early Childhood Intervention (ECI) system in Croatia is ongoing, with the National Plan for Early Childhood Intervention for 2026–2030 currently in the drafting phase.
The plan’s purpose is to establish a comprehensive, sustainable system based on intersectoral collaboration and coordination among the health, social welfare and education sectors. The drafting process is participatory and partnership-based, with extensive consultations carried out from July 2024 to July 2025. These consultations involved diverse stakeholders, including users, representatives of expert institutions and organizations, and decision-makers at all levels, to collectively identify key challenges and define priority goals for the further development of the ECI system. The initiative was launched by the UNICEF Office in Croatia, providing expert and technical support throughout the process. The Ministry of Health led the activities and coordinated the process, while the Centre for Health Systems, Policy and Diplomacy at the University of Zagreb’s School of Medicine provided expert and technical support. Stakeholders involved in the consultation process included those directly or indirectly engaged in decision-making, planning, organization and service delivery within the ECI system.
The rationale for the National Plan arises from challenges and gaps in the current system for children aged 0 to 7 years. UNICEF’s 2020 analysis highlighted fragmentation, lack of strategic coordination, uneven availability and limited institutional capacity in Croatia’s ECI system. Currently, there is no unified national strategic or legislative framework systematically regulating early intervention. Instead, relevant services are governed by multiple sectoral laws, with differing definitions and operationalizations by the health, social welfare and education sectors. This fragmentation hampers recognition of ECI as an integrated, intersectoral system critical for optimal child development.
The Ministry of Health, in cooperation with county authorities and health centres, is establishing a network of mobile clinics that will serve nearly 80% of Croatia’s rural, remote and island communities. At the same time, a new system of mobile pharmacies is being launched.
As part of the initiative, physicians and nurses operating from specially equipped mobile healthcare units will visit small and isolated communities where access to health services has previously been limited or unavailable. These mobile teams will provide basic medical care, prescribe treatments, issue referrals and prescriptions, and conduct home visits for immobile patients.
The project will enhance access to care for older people and individuals with reduced mobility. A total of 33 vehicles will be procured and distributed across the counties to support this effort. The total investment for this component amounts to EUR 5.3 million, with an implementation period of 14 months.
In parallel, mobile pharmacies are being rolled out as part of the broader initiative. The mobile pharmacy units (equipped camper vans with appropriate pharmaceutical equipment and digital systems) will be deployed in Lika-Senj, Karlovac, Sisak-Moslavina, Brod-Posavina, Vukovar-Srijem and Zagreb counties. Two pharmacy boats will operate in Zadar County to serve surrounding island populations.
The Ministry of Health has signed a formal agreement with counties and pharmacy institutions to implement the mobile pharmacy service within the framework of the National Recovery and Resilience Plan 2021–2026, with a dedicated budget of EUR 3 million. The main objective is to ensure the regular supply of medicines and pharmacy services in locations without direct access to a permanent pharmacy.
References
For more information (in Croatian) see:
In July 2023, the Ministry of Health announced a reform measure that reduces the administrative burden on primary care physicians, which includes family physicians, paediatricians and gynaecologists.
After evaluating processes in primary healthcare, the Ministry of Health and the Croatian Health Insurance Fund (CHIF) identified challenges, including an administrative overload of physicians. Several processes have now been transferred from doctors to the administrative services of the CHIF, including the procedure of checking and deciding on the justification of issued travel vouchers, as well as requests of insured persons for reimbursement of transport costs. This reform aims to enable doctors to better devote themselves to patients, which is also the focus of the comprehensive health system reform.
In addition to reducing the administrative burden, the government and the health administration aim to respond to other challenges in primary healthcare through a series of reform measures. These include financing the specialization of 922 doctors at a cost of EUR 130 million (including the specialization of 147 doctors in primary healthcare–related specialties), equalizing the coefficients of hospital specialists and specialists in primary healthcare, specialist training of nurses in the field of emergency medicine, strengthening the coordination role of the health centre, strengthening the primary healthcare infrastructure, reorganizing the emergency medical service, merging of ambulance and emergency medicine, establishing nursing counselling centres to provide basic care for certain chronic diseases, and introducing psychological and speech therapy as well as physical therapy at health centres.
References
More information is available (in Croatian) at:
On 24 May 2023, the State Audit Office issued a report on the audit it conducted on the effectiveness of primary health care in Croatia.
The subject of the audit was the activities of the Ministry of Health, the Croatian Institute for Health Insurance and the Croatian Institute for Public Health related to the planning and availability of doctors and the territorial coverage of public health services of primary health care providers in the field of family medicine, women’s health and preschool children’s health.
Based on the findings of the audit, the State Audit Office concluded that family medicine, women’s health care and health care for preschool children were only partially effective.
The State Audit Office issued the following orders and recommendations:
- Considering that the Strategic Plan for the Development of Human Resources was adopted for the period until 2020, a new Strategic Plan for the Development of Human Resources should be developed, which should consider the estimated size of the health workforce, existing job categories, and the required number of specialists.
- A central body responsible for human resource management in the health system should be established, with responsibility for strategic planning and human resource management.
- The Ordinance on personnel standards for teams at the primary healthcare level should be adopted, in accordance with the provisions of the Health Care Act.
- The Network of Public Health Services should be established in accordance with the provisions of the Health Care Act.
- For the purpose of unifying data for monitoring human resources and making decisions on human resource planning in health care, the National Register of Health Care Providers should be established and the Ordinance on maintaining the National Register of Health Care Providers in accordance with the provisions of the Health Care Act should be adopted.
- Reasons for the decrease in the number of doctors in family medicine, women’s health and preschool children’s health should be determined.
- Activities aimed at ensuring a sufficient number of doctors in the fields of family medicine, women’s health and preschool children’s health should be proposed.
- The content of the Catalogue of Information Standards in Healthcare should be determined in accordance with the provisions of the Act on Data and Information in Healthcare.
- The National Public Health Information System should be connected with other public information systems in order to enable the collection of quality data for planning the number of doctors in the fields of family medicine, women’s health and preschool children’s health.
- For the purpose of determining the availability of doctors in the fields of family medicine, women’s health and preschool children health, comprehensive long-term data on human resources should be collected and analyzed.
- In order to improve the planning of specializations, a single record should be organized and maintained that contains:
- information on the name and date of the document on the basis of which specialization approval was requested;
- a comparison of requested and approved specializations according to the plan;
- reasons for approval or rejection of specialization;
- name and date of the document by which the requested specialization was approved or rejected;
- sources from which specializations are financed; and
- data on completed specializations, withdrawal from specialist training and the effects of implementing specialist training and other data.
- Annual plans for necessary specializations of health workers should be adopted, based on the National Plan for Specialist Training, in accordance with the provisions of the Health Care Act.
The State Audit Office holds that the implementation of these orders and recommendations would help to address current shortcomings and improve the availability of family medicine, women’s health care and health care for preschool children in the public system.
References
For more information (in Croatian) see:
A pilot project of preventive health examinations was launched in April 2023, covering five counties: Osijek-Baranja, Sisak-Moslavina, Međimurje, Primorje-Gorski Kotar, and Split-Dalmatia.
The pilot project will last four months. A total of five health centres, or 364 family medicine teams, will have the opportunity to participate in the project. The examinations will cover 1,000 people over the age of 40 years who have not seen their family doctor for at least two years. Patients will receive invitations from the Institute of Public Health by post, email or phone call, and will receive a paid day off for the day of examinations. The preventive programme is completely voluntary for both patients and family medicine doctors.
After the pilot project ends in July 2023, an evaluation will be undertaken in September 2023. The implementation of the project at the national level is planned to start in October 2023.
References
For more information (in Croatian) see:
https://zdravlje.gov.hr/vijesti/prvi-preventivni-pregledi-krecu-pocetkom-svibnja/6019
The Ministry of Health hosted a meeting of the Working Group tasked with proposing solutions for addressing primary healthcare challenges arising from the increasing number of third-country nationals coming to work in Croatia. The meeting was attended by representatives from diverse institutions, including the Ministry of Health, the Croatian Institute of Public Health, the Ministry of Foreign and European Affairs, the Ministry of the Interior, and other relevant institutions.
Key topics included overcoming language barriers, managing potential epidemiological risks, and addressing other critical public health and safety challenges in Croatia. The discussions also covered potential amendments to regulations on medical examinations for foreign workers and changes to the Law on Protecting the Population from Infectious Diseases.
The initiative was spearheaded by the Association of Family Medicine Practitioners (in Croatian: KOHOM), which highlighted challenges in providing health services to foreign workers, such as language obstacles and the lack of comprehensive medical histories.
References
For more information (in Croatian) see: