-
13 February 2025 | Policy Analysis
First speech therapy act in Croatia adopted by the government -
24 November 2024 | Country Update
Speech Therapy Act under public consultation -
09 October 2024 | Policy Analysis
Action Plan for Obesity Prevention 2024–2027 -
19 March 2023 | Policy Analysis
The new Health Care Act -
21 October 2022 | Country Update
Introduction of electronic health records in hospitals -
10 September 2022 | Country Update
Accreditation of hospitals -
08 February 2022 | Policy Analysis
National Plan for the Development of Social Services for the period 2021–2027 -
01 February 2022 | Policy Analysis
The new National Health Development Plan for the period 2021–2027
6.1. Analysis of recent reforms
Table6.1 shows major health reforms which have been undertaken since 2013.
Table6.1
On 6 February 2025, the government adopted the proposal for the first speech therapy act in Croatia.
The law will regulate the issuance of licenses for independent practice, organizational forms of work, duties and responsibilities of speech therapists. In addition, it introduces professional supervision over their work, which is hoped to improve the control of the quality of services provided and ensure a safer, more efficient and more accessible support system for patients requiring speech therapy.
One of the key segments of the law is the establishment of the Croatian Chamber of Speech Therapists, initiated by the Ministry of Health and the Croatian Speech Therapy Society. The chamber will have public authority, including the issuance, renewal and revocation of licenses for independent practice, maintaining the register of speech therapists, conducting professional supervision and recognizing foreign professional qualifications in accordance with regulations on regulated professions.
The adoption of this law aligns with the goals of the National Health Development Plan 2021–2027, which emphasizes strengthening primary healthcare and increasing the availability of speech therapy services within the Public Health Network.
Reactions from the profession
The Croatian Speech Therapy Society welcomes the adoption of this law, highlighting its importance in addressing the serious shortage of professionals in this field. While the majority of professionals are concentrated in Zagreb, many counties (such as Lika-Senj, Šibenik-Knin and Dubrovnik-Neretva) face a significant shortage of staff. In addition to contributing to a more even distribution of professionals, the law is hoped to ensure the necessary regulation of the profession, ending irregular practices and ensuring high professional standards in providing speech therapy.
For more information (in Croatian) see:
The Ministry of Health initiated a public consultation on the draft proposal of the Speech Therapy Act, aimed at improving the quality and accessibility of speech therapy services. The new law responds to the growing need for professional support for individuals with speech and language disorders, especially in children, and aligns national legislation with European standards.
The law seeks to ensure high standards in the provision of speech therapy care, while also regulating the issuance of permits for independent practice, organizational work models, duties and responsibilities of speech therapists, and professional oversight of their work.
Under the new law, speech therapy services will be available at the primary healthcare level, and, for the first time, the public healthcare network will allow the contracting of speech therapists within health centres, where the service can be provided without a referral.
References
For more information (in Croatian) see:
Obesity is a major public health issue in Croatia. In 2019, nearly two-thirds of adults (64.8%) were overweight (body mass index equal to or over 25) or obese (body mass index equal to or over 30) and Croatia was with Malta among the two countries with the highest share of adults with overweight or obesity.
In March 2024 the Croatian government adopted the Action Plan for Obesity Prevention for the period 2024–2027. The document emphasizes that obesity is a complex multifactorial disease but also a major risk factor for the development of other chronic non-communicable diseases such as Type 2 diabetes, cardiovascular diseases and some types of cancer. Besides impaired physical health, people with obesity often face stigmatization that can affect their mental health. Since overweight and obesity often start at an early age, timely action is key to prevention, taking into account age (pregnancy and newborn, children and young people, adults and elderly) and life habits by age groups (eating habits and physical activity).
The objective of the document is to reduce the burden of obesity by taking measures for promoting healthy lifestyles and preventing risk factors and for the recognition, monitoring and treatment of obesity. The main outcome indicators are the share of overweight and obese adults (64%) and children (35%), with the goal that the numbers remain the same in 2027.
General measures for all age groups are:
- Promotion of physical activity,
- Promotion of healthy eating habits,
- Support for the development of a non-obesogenic environment,
- Education,
- Support and treatment of persons with obesity (through counselling centres and centres for obesity treatment)
- Centralized coordination, development and dissemination of evidence-based practices in obesity prevention
Additional specific measures are anticipated for certain age groups, including pregnancy, children and adolescents, adults and older people.
The main institutions charged with implementation of the Action Plan are the Croatian Institute of Public Health and the Ministry of Health, which is responsible for multisectoral cooperation (such as with the Ministry of Science and Education, the Faculty of Kinesiology, medical associations, and local government).
Regarding the funding of anticipated activities, the action plan has estimated annual financial resources, by activities, for the period 2024–2026, but some institutions, such as the Ministry of Health, will work on the plan within their regular activities, without additional funds.
References
On 17 March 2023, the Croatian Parliament accepted Amendments to the Health Care Act as part of the ongoing health reform.
The amended Health Care Act introduces new concepts such as:
- Integration of care (across levels of health care, as well as between health and social care), which will later be specified in a rulebook on integration.
- The complex patient, understood as a patient who suffers from mutually aggravating conditions. Patient complexity is seen as consisting of medical, socioeconomic, and/or psychological factors specific to the person that interfere with the provision of usual care and decision-making regarding a patient’s condition.
- A 24/7/365 care model, referring to the provision of comprehensive, continuous and coordinated care in different settings and from different care providers for the entire duration of the health need taking into account social needs as well.
- A hospital without walls concept that includes care provision, management, and monitoring, regardless of the health care setting and including hospitals, nursing homes, and home care.
Moreover, the new Health Care Act aim to strengthen primary health care by:
- establishing one health centre per county and strengthening its role as the fundamental provider of primary health care;
- strengthening the coordination and integration of long-term care activities within the health centre and with other stakeholders in health care, social care, as well as patients and their caregivers; and
- strengthening specialized secondary-level care outside of hospitals and within health centres.
This aims to provide easier access to health services, reduce the burden on the hospital system, and shorten waiting times.
Third, the amendments aim to strengthen the hospital system and improve their management by transferring ownership of general hospitals from counties to the state. This change aims to achieve financial sustainability by strengthening business control mechanisms at the national and regional level, and increasing skill requirements for the management teams of health institutions.
For more information on the Health Care Act (in Croatian) see:
As part of the introduction of new digital tools in healthcare, the electronic health record (“eKarton” in Croatian) has been introduced in 25 hospitals in Croatia. It is a technological solution that consolidates data for each patient, including details of medical examinations, diagnoses, referrals, discharge letters and issued prescriptions.
The tool enables communication between hospitals, and the discharge letter and diagnoses can be shared between all healthcare stakeholders in primary care and hospitals. The electronic health record also contains information on chronic conditions, allergies, vaccination records and the current treatment regimen. It is accessible to patients through a Health Portal (“Portal zdravlja” in Croatian), which is an integral part of the e-Citizens portal. By using the Health Portal, patients can retrieve some of their own medical data (for example, the list of prescribed medications, laboratory results) and can also communicate with doctors at the primary care level (for referrals, ordering examinations, etc.).
There are plans to expand the electronic health record to other hospitals, which is hoped to improve doctors’ understanding of patients’ general condition and health status, facilitate the administrative part of the work, enable a more efficient use of resources, reduce waiting times, and provide patients with a higher standard of health services and better interaction with the health system.
For more information (in Croatian) see: https://www.index.hr/vijesti/clanak/ministarstvo-zdravstva-ekarton-u-primjeni-u-25-bolnica/2405818.aspx
After the merger of the Agency for Accreditation and Quality in Healthcare with the Ministry of Health in 2019, the establishment of a hospital accreditation system has been resumed: 15 hospital institutions of different levels throughout Croatia were selected for the accreditation procedure. The aim is to improve the monitoring of quality and efficiency indicators, and increasing the capacity for quality system development. The project is financed through the European Social Fund programmes.
For more information (in Croatian) see:
The Ministry of Labour, the Pension System, Family and Social Policy created the National Plan for the Development of Social Services for the period 2021–2027. It is a medium-term strategic plan that is aligned with the National Development Strategy until 2030, the European Commission’s Cohesion Policy Guidelines for the period 2021–2027, and other international documents specifically related to certain population groups (for example children, people with disabilities, or female victims of violence).
The Plan aims to ensure an equal availability of social services across the country. The emphasis is on socially vulnerable groups. The National Plan for the Development of Social Services for the period 2021–2027 determines the priorities for the development of social services, as well as the needs for different forms of care (institutional and non-institutional), with the aim of achieving a systematic plan of care aligned with the needs of users. This includes increasing the quality and improving the monitoring of the provision of social services. The Plan was adopted by the Government in December 2021.
The National Plan for the Development of Social Services for the period 2021–2027 encompasses two priorities in the area of social services development:
- Availability and balanced regional development of social services;
- Quality and sustainable development of social services.
Within each priority, specific goals have been established.
Priority 1: Availability and balanced regional development of social services
This priority area refers to the elimination and reduction of regional inequalities in the provision of social services by ensuring a wider scope of social services and developing new services for the purpose of meeting the needs of socially vulnerable groups, supporting life in the community and preventing social exclusion of individuals. This Priority includes two specific goals:
- Increasing the availability of social services
- Introducing new services (social innovation).
Priority 2: Quality and sustainable development of social services
This priority area refers to the improvement of social service management and the strengthening of the capacity of social service providers. This priority includes two specific goals:
- Improving the management of social services
- Strengthening the capacity of social service providers.
The goals established in the National Plan for the Development of Social Services for the period 2021–2027 will be implemented through measures defined in Action Plans. The allocation and availability of financial resources for the implementation of individual measures, sources of funding and planned funds per year will be presented in more detail in the Action Plans. For the seven-year period of implementation of the National Plan for the Development of Social Services 2021–2027, two Action Plans will be drawn up, which will contain detailed measures and planned financial resources: an Action Plan for the Development of Social Services for the period 2021–2024 and an Action Plan for the Development of Social Services for the period 2025–2027. The Government has so far adopted the Action Plan for the Development of Social Services for the period 2021–2024.
Financial resources for the implementation of the National Plan for the Development of Social Services for the period 2021–2027, that is, the measures specified in the accompanying Action Plans, will be provided primarily from the State Budget and from European funds for the period 2021–2027.
The coordinator of the implementation of the National Plan for the Development of Social Services for the period 2021–2027 is an internal organizational unit of the Ministry of Labour, Pension System, Family and Social Policy in charge of strategic planning.
References
For more information (in Croatian) see:
- https://mrosp.gov.hr/UserDocsImages/dokumenti/Glavno%20tajni%C5%A1tvo/Godi%C5%A1nji%20planovi%20i%20strate%C5%A1ka%20izvje%C5%A1%C4%87a/Nacionalni%20plan%20razvoja%20socijalnih%20usluga%20za%20razdoblje%20od%20%202021.%20do%202027.%20godine.pdf
- https://narodne-novine.nn.hr/clanci/sluzbeni/full/2021_12_136_2240.html
- https://narodne-novine.nn.hr/clanci/sluzbeni/2021_12_147_2536.html
The National Health Development Plan for the period 2021–2027 was adopted by the Government of Croatia on 30 December 2021. It is aligned with the National Development Strategy until 2030, the Government Programme, the National Recovery and Resilience Plan for 2021–2026 and the European Commission’s Cohesion Policy Guidelines for the period 2021–2027. It is a medium-term strategic plan that establishes specific goals, measures, projects and activities that will be implemented under the auspices of the Ministry of Health with the overarching aim of improving the health system and population health outcomes.
The National Health Development Plan for the period 2021–2027 comprises five specific goals:
- Improved healthy lifestyles and more effective disease prevention;
- Improvement of the health system;
- Improvement of the model of care for key health challenges;
- Making the health system a desirable place to work;
- Improving the financial sustainability of the health system.
1. Improved healthy lifestyles and more effective disease prevention
In order to achieve goal number 1, six measures have been outlined:
- Promotion of healthy lifestyles
- Prevention of leading non-communicable diseases, including caries, injuries and mental illnesses
- Prevention of priority infectious diseases
- Prevention of disability caused by the most common risk factors
- Prevention of diseases caused by the harmful effects of environmental factors
- Establishment of digital solutions in the health information infrastructure to promote disease prevention and healthy lifestyles
2. Improvement of the health system
In order to achieve goal number 2, twelve measures have been outlined:
- Strengthening horizontal and vertical integration of primary health care
- Coordination and integration of health and social care resources
- Modernization of hospitals and functional integration of health institutions
- Re-establishment of the Immunology Institute
- Establishment of excellence centres
- Establishment of a framework for measuring the effectiveness of health services
- Introduction home haemodialysis
- Establishment of a comprehensive national system of health care quality and safety
- Improvement and development of health tourism
- Strengthening health technology assessment
- Development of systems for more efficient emergency care and transport of patients or health resources, including helicopter emergency services
- IT connection of all health service providers
3. Improvement of the model of care for key health challenges
In order to achieve goal number 3, nine measures have been outlined:
- Development of improved clinical guidelines for diseases that place the greatest burden on the health system
- Improvement of the treatment of patients with cardiovascular and cerebrovascular diseases
- Improvement of the treatment of patients with cancer
- Improvement of the treatment of patients with dementia and consciousness disorders
- Improving the availability and quality of health care for patients with rare diseases
- Capacity building in the field of diabetes care
- Monitoring and reporting of patient health outcomes at the institutional and regional level, including through patient-reported outcomes
- Establishment of digital platforms and systems for education and communication with patients
- Responses to crisis situations
4. Making the health system a desirable place to work
In order to achieve goal number 4, four measures have been outlined:
- Creation of a strategic framework for the development of human resources
- Improvement of material and working conditions of employees in the health system
- Introduction of a work evaluation system and encouragement of excellence in health care
- Specialist training of health workers and programmes of lifelong learning
5. Improving the financial sustainability of the health system.
In order to achieve goal number 5, five measures have been outlined:
- Development of a strategic framework for sustainable financing of the health system
- Improvement of the unified public procurement system
- Improvement of hospital management
- Introduction of a system for determining the prices of health services that reflect the costs of effective treatment
- Improvement of the payment model for health services
The five specific goals established in the National Health Development Plan for the period 2021–2027 will be implemented through measures defined in two Action Plans. The allocation and availability of financial resources for the implementation of specific measures, sources of funding and planned funds per year will be presented in more detail in the Action Plans. For the seven-year period of implementation of the National Health Development Plan 2021–2027, two Action Plans will be drawn up, which will contain detailed measures and planned financial resources: an Action Plan for health system development for the period 2021–2025 and an Action Plan for health system development for the period 2026–2027. The Government has so far adopted the Action Plan for health system development for the period 2021–2025.
Financial resources for the implementation of the National Health Development Plan 2021–2027, that is the measures outlined in the accompanying action plans, will be provided primarily from the State Budget and from European funds for the period 2021–2027.
The coordinator of the implementation of the National Health Development Plan 2021–2027 is an internal organizational unit of the Ministry of Health in charge of strategic planning.
References
6.1.1. Financing
Financing of the CHIF
Between 2002 and 2015 funds allocated for health care were determined annually by the state budget and collected through the State Treasury. The CHIF received its funds from the state budget. These funds originated from three sources: contributions for mandatory health insurance, funds collected by general taxation and county funds collected from regional taxes (Voncina, Dzakula & Mastilica, 2007). In 2015 financing of the CHIF was separated from the State Treasury (as it had been in 1990–2002), which enabled it to manage earmarked funds for health care independently. Some of the benefits expected from the separation were improved transparency in health care financing, stabilization of the health care budget, more efficient cost management and the introduction of payment mechanisms that incentivize the quantity and quality of services (CHIF, 2014).
World Bank loan
In 2014 Croatia signed a Loan Agreement for over €75 million with the World Bank for the Improving the Quality and Efficiency of Health Services Programme. This Programme supported five of the eight priorities of the 2012–2020 National Health Care Strategy aimed at resolving the biggest reform challenges in the health sector, including strengthening management capacity in health care, reorganizing the structure and activities of health care institutions, improving the quality of health care, strengthening preventative activities and preserving the financial sustainability of the system (World Bank, 2014b). The Programme closed on 31 October 2019. It was rated by the World Bank as moderately satisfactory in achieving project development objectives and overall implementation progress (World Bank, 2019b).
Increase in health care revenue
A higher health insurance premium is expected to improve the financial situation of the health system. Since January 2019 the health insurance contribution rate has increased by 1 percentage point, to 16.5% of gross salary for all employees, increasing the reliance of health financing on the working population. According to official estimates, this should increase contributions by 0.4% of GDP (an increase of roughly 6% of the total revenue of the CHIF). No measures are currently planned to broaden the base of paying users beyond those in employment. Similarly, no specific plans have been disclosed to address the current stock of arrears in hospitals’ finances (European Commission, 2019a) (see below and Chapter 3).
6.1.2. Primary care
Group practices, payment by quality and performance
In 2013 several changes were introduced to the financing of primary care. In addition to the basic income (including fixed office maintenance expenses, income per insured person by age group and per DTP), additional revenue opportunities were established. These were based on specific quality and efficiency indicators, as well as for providing preventive check-ups, forming group practices and engaging in e-health services, counselling groups and phone consultations. These additional revenue opportunities can amount to 5–7.5% of the basic income (CHIF, 2013).
Abolition of concessions and introduction of private practices
With the 2019 Health Care Act the privatization of primary care has been continued through weakening the role of county health centres as key stakeholders in governing the organization of primary care for their respective population (see Chapter 5). The upper limit of primary care professionals that are employed within county health centres decreased from 30% to 25%.
Concessions, which had been given approval by the local or regional authority based on the public health service network, have been turned into practices approved by the Ministry of Health, allowing providers to enter contracts with the CHIF, local or regional authorities, voluntary insurers, universities, etc. Concessions allowed for greater control over private practices in primary care, and private physicians sought to weaken this regulatory mechanism and to treat practices as their private investment.
6.1.3. Hospitals
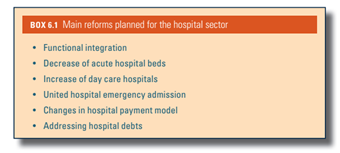
The National Hospital Development Plan was adopted in September 2018. Building on a previous document for 2015–2016, it sets out “functional integration” as one of the main principles in facilitating the modernization and restructuring of hospitals, as well as in improving quality of care (see Box6.1). The process was initiated in 2017, but no official report detailing the content or the progress of implementation has been published so far. Furthermore, this reform of the hospital system does not take full consideration of the parallel initiatives in strengthening outpatient care. The two processes do not appear to be well coordinated, posing the risk of unsatisfactory outcomes (European Commission, 2019a). Functional integration envisages the integration of hospitals within five regions (Central (including the city of Zagreb), North, East, West and South), reorganizing them according to modality of care: day care, acute care and long-term care hospitals. The reorganization aims to emphasize day care hospitals and decrease acute care capacities in favour of chronic care, long-term care and palliative care capacities. Emergency hospital care departments are planned to be centralized within a hospital as opposed to each department (i.e. internal medicine, neurology, surgery, etc.) having separate emergency entrances. It is hoped this will contribute to horizontal integration with the outpatient emergency service and overall better care for emergency patients (Ministry of Health, 2018b).
Box6.1
In 2015 the CHIF started paying hospitals part of their monthly revenue upfront and disbursed the remainder after the services had been delivered. Since 2020, 100% of hospital income has been paid in advance (up from 90% in 2019) and the hospitals then provide invoices based on episodes of care. The payment model introduced since 2015 also involves monitoring five quality and efficiency parameters. Since the introduction of these changes hospitals appear to have reduced average length of stay, increased provision of day care and same-day surgery, increased the number of outpatients in specialist care and increased the number of surgical operations and procedures performed. The new model was also hoped to lead to improvements in quality of care, but it is currently not possible to measure whether this aim has been achieved, as quality management systems in hospitals are only starting to be developed (Poslovni dnevnik, 2015).
Some hospitals in the country provide services in excess of the limits set by the CHIF, while others maintain capacities greater than the needs of the population they serve. While the authorities have announced plans to increase the spending limits for hospitals across the board, the system is likely to remain prone to accumulation of arrears, as long as the spending limits are not brought closer in line with the types and amounts of services provided in each of the hospitals (European Commission, 2019a).
Priority waiting lists
In 2017 the Ministry of Health introduced a new management system for hospital waiting lists, called “priority waiting lists”. The new system started for several months as a pilot programme in four hospitals in Zagreb, and was then implemented nationwide. It has been designed for patients who are suspected of suffering from a serious illness, such as a tumour, which, although not immediately life-threatening, necessitates accelerated diagnosis and treatment. Some 10% of places on the existing waiting lists are reserved for priority patients with suspected serious illness. Patients on priority waiting lists are referred to a specialist by their GP. The specialist consultation is to take place within one week of the referral. Priority waiting lists are implemented in 27 acute hospitals, while in others the implementation is still ongoing. Priority referral justification analysis has shown that over 92% of referred patients required priority diagnostics and treatment (Brekalo, 2017; Government of the Republic of Croatia, 2019; Ministry of Health, 2020b).
6.1.4. Public health
E-health solutions
In 2014 the Croatian Government launched the e-Citizens portal, enabling citizens to communicate with the entire state administration system via a personalized electronic mailbox. With regard to health care, citizens can access information on their chosen primary health care physicians, request a European Health Insurance Card, retrieve information on filled drug prescriptions, their e-orders and available dates for health care services, as well as information on their health insurance policy status (CHIF, 2020b).
E-health solutions have the potential to improve the efficiency of the health system in Croatia. E-prescriptions have been successfully introduced and are fully operational. E-referrals and electronic health records are still under development. Planned investment in equipment in health centres is expected to improve the system’s capacity for the further development of e-health services (European Commission, 2019a).
The Law on Health Data and Information
In 2019 the Croatian Parliament adopted the Law on Health Data and Information. The law sets out a legal framework for the use and management of health data and information and for quality assurance at the national level (Republic of Croatia, 2019a).
Central Management System
In 2019 the Central Management System was formally introduced as the new IT support system for managing the organizational structure of health care providers, particularly hospitals. The system was established by the Ministry of Health in cooperation with the CHIF and the CIPH. It is seen as a qualitative step forward in the exchange and analysis of hospital and public health data and builds on the data exchange established by the Central Health Information System (see section 2.6). The main objectives of establishing a Central Management System are to gain a better central oversight over the organizational structure of health care institutions, allow the creation and distribution of notifications, have a better overview of the supply of pharmaceuticals, and increase the transparency of hospital spending and effectiveness (Tomic, 2019).
Rationalization of public health and health quality agencies
With the 2019 Health Care Act and the Act on Quality in Health Care, the Institute for Health Protection and Safety at Work and the Institute of Toxicology and Anti-Doping have been merged into the CIPH, while the Agency for Quality and Accreditation in Health Care has been merged into the Ministry of Health (Republic of Croatia, 2019b, 2019c).
6.1.5. Human resources
Strategic Plan for Human Resources
In 2015 the Government adopted the Strategic Plan for Human Resources in Healthcare for 2015–2020. The Plan recognizes that one of the fundamental problems in the area of human resources development in the Croatian health system is the lack of a human resources management system. A comprehensive system for monitoring human resources in the health system is needed in order to improve projections of supply and estimates of needs (both in terms of numbers and types of health professionals). The Plan envisages the development of a system for the organization and active management of human resources in the health sector with the aim of achieving a sufficient and adequate staff structure. Implementation has been limited so far, with no available information on progress achieved.
In 2018 HRK 82.2 million in grants was awarded within the Operational Programme for Efficient Human Resources for Croatia in 2014–2020, funded by the European Social Fund. The primary goal of this grant has been to improve access to primary care in deprived parts of Croatia by financing the training of 76 specialists in family medicine, paediatrics, clinical radiology, emergency medicine and gynaecology and obstetrics in those areas (Ministry of Health, 2018a).
6.1.6. Access to expensive medicines
Apart from the CHIF’s fund for very expensive drugs, whose revenue has been increasing markedly over recent years, in 2017 the Government established a fund for very expensive drugs to which private donations can be made, in order to finance very expensive drugs that are not covered by the CHIF.6.1.7. Palliative care
The 2014–2016 Strategy for Palliative Care has been extended for the 2017–2020 period. The strategies greatly enhanced capacity for palliative care by improving integration and coordination, rather than developing new structures. Guidelines have been adopted and palliative care services established in inpatient and outpatient settings. Several county-level palliative care plans have been adopted, in accordance with the 2017–2020 strategy. The strategy is continuously implemented and shows measurable results.6.1.8. Reforms which failed or were passed but never implemented
Hospital restructuring to achieve greater functional integration has not been implemented and, except for a few cases of hospital mergers, it is not possible to determine how far the strategic plan has been achieved. Likewise, the issue of hospital debts has not been addressed, but continues to be discussed between the central Government (the Ministry of Health, CHIF and the Ministry of Finance) and hospitals.
The envisaged human resources management system has not been developed at the time of writing (April 2021), and although the number of medical residents has increased, it is not possible to identify a systematic human resource management policy in any other segment of health care.

