-
28 May 2025 | Country Update
An increase of quotas for physicians and dentists -
02 September 2024 | Policy Analysis
Creation of new roles and profiles to improve the attractiveness of primary care professions -
05 June 2024 | Country Update
Advanced practice nurses: A Royal Decree to define their competencies -
10 August 2020 | Policy Analysis
Adaptations of the quota system for physicians
4.2. Human resources
The COVID-19 pandemic severely affected health professionals, and improving the attractiveness of the health professions was an important focus in 2024, with the creation of new roles and profiles to support nurses and general practitioners (GPs).
Since the extension of nursing studies in 2016, a distinction has been made between nurses responsible for general care, who must have completed a four-year programme (bachelor level), and nursing assistants, who must have completed a three-year programme. A royal decree of September 2023, amended in April 2024, defines the list of nursing services that can be provided by a nursing assistant, as well as their conditions of practice. In less complex situations, the nursing assistant can work independently within the limits of their competence, but in more complex situations, the nursing assistant works under the responsibility of a nurse or a doctor.
The qualified caregiver has also been recognized since February 2024. A qualified caregiver is a person who is not a nurse, but who is authorized, within the framework of their professional or voluntary activity, to provide well-defined care services outside a care institution (in a school, crèche, day centre, institution for the disabled or at home). These are simple care services, such as administering insulin to a person with diabetes. Written authorization from a doctor, nurse or nursing assistant is required. The authorization defines what the qualified carer can do and under what circumstances, and also ensures that the necessary training and instructions are provided.
In April 2024, two royal decrees also defined the clinical activities and medical procedures that advanced practice nurses may carry out, as well as the criteria for recognition as an advanced practice nurse.
The recognition of the clinical research nurse is also in progress. This is intended to cover nurses with a doctoral degree who work in collaboration with universities and/or organizations with a scientific background.
To support GPs, the title of practice assistant has also been recognized since May 2024. These paramedical professionals assist GPs with administrative tasks as well as some technical support tasks (such as taking samples for the laboratory or taking the weight), under the supervision of the physician. A specific training programme has been defined in 2023 (90 ECTS or 970 hours). Moreover, since September 2024, GP practices have been able to apply for a financial contribution to conclude an initial employment contract with a practice assistant or a nurse.
Authors
References
FPS Public Health (2024). Nurses responsible for general care (https://www.health.belgium.be/fr/sante/professions-de-sante/infirmiers-aides-soignants/infirmiers#reglementation (in French) / https://www.health.belgium.be/nl/gezondheid/zorgberoepen/verpleegkundigen-zorgkundigen/verpleegkundigen (in Dutch)
FPS Public Health (2024). Nursing assistant (https://www.health.belgium.be/fr/assistant-en-soins-infirmiers (in French) / https://www.health.belgium.be/nl/basisverplegkundige (in Dutch)
FPS Public Health (2024). Qualified caregiver (https://www.health.belgium.be/fr/aidant-qualifie#Legislation (in French) / https://www.health.belgium.be/nl/bekwame-helper (in Dutch)
FPS Public Health (2024). Advanced practice nurses (https://www.health.belgium.be/fr/infirmier-de-pratique-avancee (in French) / https://www.health.belgium.be/nl/verpleegkundig-specialist (in Dutch)
FPS Public Health (2024). Practice assistant (https://www.health.belgium.be/fr/assistant-de-pratique (in French) / https://www.health.belgium.be/nl/praktijkassistent (in Dutch)
Authors
References
4.2.1. Planning and registration of human resources
Since 2014, a reform of the regulation of health care professionals has been in progress, based around three pillars: competent health care providers, integrated and multidisciplinary health care and patient-centred care.
Health care professionals are regulated and listed in a specific law (BS-MB 18 June 2015), which is regularly updated (for example, the profession of clinical psychologist was added in 2016). They are obliged to have their diploma formally registered and to obtain a visa, which is a licence to practise. The visa gives permission to exercise the profession and enter the Belgian labour market. The visas are issued by the MoH and do not expire. Notwithstanding this, in cases of malpractice, a visa can be recalled under certain conditions. A recent law on quality practice in health care, which will come into force from July 2021, creates a framework for monitoring the competences of a health care professional in a more flexible way (via an electronic portfolio) and not solely on a visa (BS-MB 14 May 2019b).
Some individual health care professionals may carry particular professional titles or refer to particular professional qualifications (for example, a title can be paediatrician and the special qualification can be competence in neonatology). To obtain these titles or qualifications, they must meet a number of criteria (such as postgraduate training or internships) before being recognized (erkennning/agrément) by the Minister of their community. For every professional title, specific criteria apply, and a special commission is set up that grants or refuses the title (BS-MB 27 May 2014). For some professions, the professional title is limited in time (which is the case for hospital pharmacists) and re-submitting an application is necessary (BS-MB 3 December 2012).
In addition to the diploma, visa and recognition of the professional title, physicians and pharmacists must be recorded in the register of the Order of Physicians or Order of Pharmacists. The Order, regulated by law, was established to safeguard the non-commercial character of the profession and was ordered to draw up a code of ethics to establish the general principles and rules that are indispensable for the exercise of the profession. The Order investigates illegal and unethical practices under its strict Code of Ethics and has the right to impose penalties and strike physicians off the register if necessary (BS-MB 14 November 1967).
An important administrative step is for health professionals to obtain approval by the NIHDI; this allows the reimbursement of their medical acts by the compulsory health insurance (namely, they obtain an NIHDI number). This individual NIHDI number is required for GPs, medical specialists, pharmacists, midwives, home nurses, physiotherapists and dentists, but is not required for insurance doctors, occupational physicians, nurses working in hospitals and residential institutions, or pharmacists working for pharmaceutical companies. Moreover, for physicians and dentists, access is limited (see Box4.3).
In line with the European legislation (European Council. 2005), individuals with a diploma from the 28 EU Member States or from Switzerland, Liechtenstein, Iceland and Norway can automatically apply for a licence. Equivalence of the diploma must be checked for others.
For people with a non-EU diploma as well as for non-EU people wishing to specialize (postgraduate training) in Belgium, there has been a stricter procedure since May 2019 and each individual application will be investigated. This new measure was put in place to help with human resource planning in light of the quota system that considers only Belgian MD diplomas (see Box4.3) (BS-MB 14 May 2019a; MoH, 2018c).
On 16 May 2025, the Council of Ministers approved the quotas for 2031 that limit the number of physicians entering specialization after their initial six-year medical training, as well as the quotas for dentists for 2030. Both quotas have been slightly increased compared to last year and previous recommendations, in order to improve healthcare accessibility and reduce waiting times for consultations.
The proposal was coordinated with the federated entities and took into account factors such as population needs, healthcare workforce demands, university training capacity and the trend of decreasing physician activity rates. The objective is to accelerate the reduction of long-standing shortages in the healthcare sector. In addition, the government has decided to take into account the impact of foreign-trained healthcare professionals when determining national quotas.
Authors
References
As described in section 4.2.1 (on Planning and registration of human resources) of the Belgian Health System Review, before the application of the sixth State Reform, access to specialisation for physicians was limited by a quota system with overall quotas defining the maximum number of physicians, stratified by community as well as minimum quotas for some specialties where a possible shortage was identified, that is, GPs or geriatricians. These quotas were determined by the Federal Minister of Social Affairs and Public Health based on the advice of the Planning Commission of Medical Supply of the MoH, which assessed the medical workforce needs, with the technical support of the Planning Unit for the Supply of Health Care Professions. Federated entities were responsible for the organization of measures to respect these quotas (for example, admission tests). Such quotas were only applied to medical graduates with a Belgian diploma and were published six years in advance so that the candidates could know them before starting their studies.
Since 2018, some changes to the quota system have occurred:
- In 2018, because the quotas have been exceeded by the French Community, the government decided to activate a smoothing mechanism aiming to resorb the surplus (1).
- The law of 29 March 2019 provides for the possibility of establishing a quota for physicians (medical graduates and specialists) with a foreign diploma and provides a two-year period to publish these quotas (2).
- Following the opinion of the Council of State of 29 July 2020, the Planning Commission of Medical Supply of the MoH is now only competent to publish advice on the overall quotas for the number of physicians per Community (3). The Planning Commission can therefore no longer issue an opinion on the minimum number of graduates in some specialties, the distribution by specialization (subquotas) being the prerogative of the Federated entities since the sixth State Reform. Due to the sixth State Reform, only overall quotas are now defined at the Federal level. There are no longer minimum quotas for some specialties. Federated entities have created their own planning commissions to manage the subquotas per specialty.
Authors
References
4.2.2. Trends in the health workforce
The Planning Commission of medical supply of the MoH publishes annual statistics on licensed health care professionals (STATAN reports) (MoH, 2017d) and more detailed trend analysis for some professions in the so-called PlanCAD reports.
Physicians
Different definitions are used to calculate the number of physicians (see Box4.4).
The overall number of practising physicians increased from 28 999 (283 per 100 000 population) in 2000 to 35 762 in 2018 (313 per 100 000 population), which is below the EU15 average (see Fig4.3 and Fig4.4). It is nevertheless important to note that the definition of practising physicians varies across countries.
| Fig4.3 | Fig4.4 |
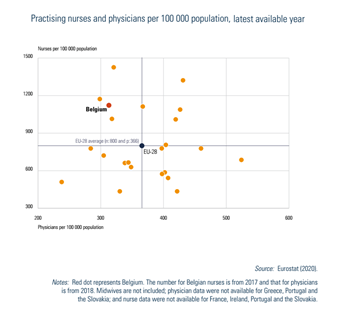 |
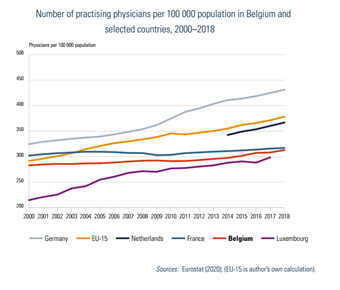 |
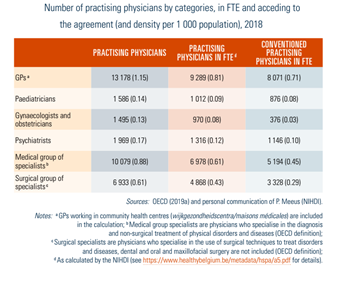
In 2018, GPs represented 37% of practising physicians, compared with 63% of medical specialists. Because in this calculation, all physicians performing more than one clinical act are considered, results are also presented in full-time equivalent (FTE) (see Table4.2, 2018 data). For Belgium, it is also interesting to report on practising physicians acceding to the agreement on NIHDI tariffs (so-called conventioned physicians).
Table4.2
It is also important to highlight that physicians in Belgium are getting older. In 2018, 44.3% of practising physicians were aged 55 years and over in comparison to 24.1% in 2000. The same is observed in other EU countries but Belgium has one of the highest shares of physicians aged 55 years and over (at around 44.3% in 2018 versus the EU15 average of 33.0%) (OECD, 2020).
This situation is especially worrying for GPs: in 2018, 52% were aged 55 years and over, which is linked to the fact that older GPs are working longer and not enough new graduates are becoming GPs to replace the retired workforce (Devos et al., 2019).
Dentists
The number of practising dentists, defined as having provided more than one clinical service during the year, has been stable since 2000 (8516 in 2017, representing 0.75 per 1000 population). Among these 8516 practising dentists, 7550 (87%) were general dentists, 180 were specialists in periodontics, 479 were specialists in orthodontics and 307 were specialists in stomatology (NIHDI, 2019k). In 2018, the title oral hygienist was legally recognized as a health profession (BS-MB 30 March 2018).
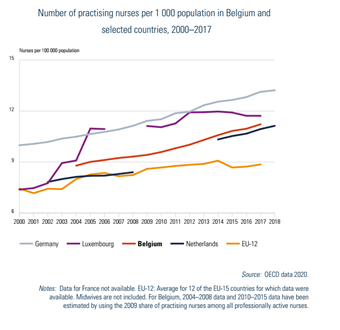
Nurses
The number of practising nurses has increased in Belgium (from 8.8 per 1000 inhabitants in 2004 to 11.2 per 1000 inhabitants in 2017). This increasing trend is also observed in other European countries. In Belgium the number of practising nurses per 1000 inhabitants is above the European average of 8.9 per 1000 inhabitants based on 12 EU countries (Fig4.5) (OECD data 2020).
Fig4.5
In 2017, there were 204 256 nurses licensed to practise, 146 094 professionally active nurses in the Belgian labour market, and 127 681 practising nurses in the health care sector (62.5% of the nurses licensed to practise) (OECD data 2020). In 2017, 84% of practising nurses worked as employees, 8% as self-employed nurses, and 8% as both. Most employed practising nurses worked in the hospital sector (66%) (MoH, 2020a).
Recent initiatives such as the creation of advanced practice nurses are described in Box4.6. More details on the nursing profession and on the available specialties can be found in Rafferty et al. (2019).
Other health care personnel
In Belgium in 2017, 13 436 midwives were licensed to practise, of which 58% were practising in the health care sector. Among professionally active midwives (n = 9757), most are employees (79.53%), 8.62% are self-employed and 11.85% have mixed status. Most self-employed midwives deliver care at home and not in hospital (prenatal and postnatal care) (MoH, 2020b) and this group is increasing over the recent years. Overall, the supply of midwives is considered high in relation to the needs of the Belgian population (65.35 practising midwives per 1000 live births in 2017, compared to an EU average of 38.06 based on 11 of the EU15 countries) (OECD, 2020a).
In 2016, the number of physiotherapists licensed to practise was 38 807, of which 59% were practising in the health care sector. Most of them are active as self-employed physiotherapists (57%), 23% as employees (in hospitals, revalidation centres, nursing homes) and 20% have mixed status (MoH, 2019e).
In 2018, there were 14 280 practising pharmacists (working in community and in hospital pharmacies), with a density of 1.25 pharmacists per 1000 inhabitants, which shows that Belgium has a high density of pharmacists (compared with an EU average of 0.86 per 1000 inhabitants based on 10 of the EU15 countries; for more details see Section 5.6 Pharmaceutical care) (OECD, 2020a).
Additional statistics on other health care professionals can be found in the STATAN reports of the MoH (https://organesdeconcertation.sante.belgique.be/fr/documents/hwf-statan-2019) and on the website of the NIHDI (https://www.inami.fgov.be/fr/statistiques/soinsdesante/2018/Pages/default.aspx).
More details on health workers distribution can be found in Box4.5.
4.2.3. Professional mobility of health workers
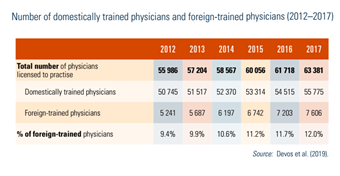
Table4.3 shows that the proportion of foreign-trained physicians in Belgium is increasing, from 9.4% in 2012 to 12% in 2017, but is still below the average of 13.9% in 2017 (based on 10 European countries). This includes licensed physicians, which does not imply that they are practising in the Belgian health care system. In 2017, half of all foreign-trained physicians came from France (18%), Romania (17%) and the Netherlands (16%) (OECD, 2019a). In 2019, a new law installed a quota for non-EU foreign-trained physicians (see Section 4.2.1 Planning and registration of human resources).
Table4.3
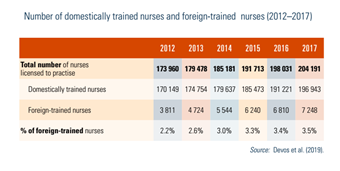
Among all nurses licensed to practise in Belgium, the share of foreign-trained nurses has been increasing over time (from 0.5% in 2000 to 3.5% in 2017) and is in line with the EU average. Concerning nationality, 13% of practising nurses in the French community have foreign nationality, mostly from France (6.6%), compared with 2% in the Flemish community (MoH, 2019d). Table4.4 shows the number of domestically trained and foreign-trained nurses in Belgium.
Table4.4
4.2.4. Training of health personnel
The organization of education is a competence for the Federated entities and therefore some training aspects may differ between communities. Most educational standards comply with EU Directive 2005/36/EC on the recognition of professional qualifications on the basis of harmonized minimum training requirements (see Box4.6) (European Council, 2005; BS-MB 18 June 2015). To improve the quality of care, continuing training is also encouraged (see Section 2.4.2).
4.2.5. Physicians’ career paths
In the hospital setting, most physicians are self-employed. Physicians in university hospitals and in some public hospitals are salaried. To be authorized as a hospital physician, the hospital legislation provides in article 145 of the Hospital Act the need to conclude a written agreement of rights and obligations between the hospital and the physician (these often include agreements on out-of-office hours) (Justel 7 November 2008). In most hospitals, physicians form an association with other self-employed physicians of a similar discipline in the same hospital. They pool their resources within this association and have individual financial agreements with the hospital board. Therefore, it is not that common for these physicians, who engage in a formal association with a contract and often a non-competition clause, to change their work environment.
In a hospital, the medical activity is hierarchically structured according to three levels (Article 18–22, Chapter 3 of the Hospital Act; Justel 7 November 2008). At the top, there is the chief medical director, responsible for all aspects of patient care, especially for medical care, paramedical and nursing care and medication, as well as for the promotion and evaluation of the quality of care provided. The chief medical director is part of the hospital board and works closely with the hospital manager. For this function, remuneration from the government is provided in the hospital budget. Next, there are the department heads, who are responsible for coordination and organization of the services, functions or care programmes entrusted to them. The chief medical director, as well as the heads of departments, are chosen by the board of directors after consulting the medical council. Then, there is the medical staff, which is formed of all hospital physicians.
The Hospital Act also specifies the installation of a medical council, consisting of physicians elected by the other hospital physicians. The medical council has an advisory function with a focus on promoting quality and cooperation (Article 132–142 of the Hospital Act; Justel 7 November 2008).
In ambulatory care settings, almost all physicians are self-employed. Group practices joining together two or more physicians are becoming more popular (in 2011, 30% of GPs in FTE worked in a group practice and in 2016, this percentage increased to 40%; NIHDI data, personal communication of P. Meeus). The vast majority of young GPs prefer to work in a group practice after their training (Missinne et al., 2018). There are also a small number of salaried GPs who work in community health centres with a capitation-based remuneration system, in homes for older people and in nursing homes.
4.2.6. Other health workers’ career paths
In hospitals, nursing activity is structured as follows: the director of nursing is responsible for the proper functioning and coordination of the nursing department, but often also of paramedical workers and psychologists. They are selected by the hospital board on the advice of the hospital manager and the chief medical director. For several departments, a head of nursing is appointed, and every nursing unit also has a head nurse. The nursing staff in hospitals includes hospital nurses, nurse assistants and carers (Article 23, Chapter 4 of the Hospital Act; Justel 7 November 2008).
Concerning training and qualifications, making the change from a diploma-level nurse to a bachelor-level nurse is encouraged and special educational packages are available. Particular professional qualifications and professional titles were financially stimulated, with an annual lump sum until 2018, but since then the system was stopped for newly hired nurses and a project to integrate this annual lump sum into an adapted wage scale with increased remuneration for the particular professional titles and professional qualifications (scale of the Institute for Functions Classification) is under discussion. Moreover, in 2019, the profession of advanced practice nurse received legal status, which will introduce new career opportunities for those who want to combine science and clinical practice (Chambre des représentants de Belgique, 2019). Nevertheless, the job description and fees are still undefined.
Efforts have been made to increase the attractiveness of the nursing profession; for example, with the attractiveness plan in 2011 and extra measures in 2013 (Gerkens & Merkur, 2010). The communities have also initiated action plans to enhance the attractiveness of some health professions (Belche et al., 2019). Nevertheless, recruiting and retaining nursing professionals remain a challenge, and difficulties persist.