Context
The “essential levels of assistance” (LEA in Italian) define the healthcare services that the National Health Service (NHS) is required to guarantee to all citizens, ensuring equitable and uniform access across the entire country. These services are evaluated based on indicators measuring the quality and effectiveness of care across three macro-areas: hospital services, district (community, primary) care, and prevention. Indicators are based on a scale of 0 to 100, with a score of 60 corresponding to the minimum guarantee threshold (that is, “sufficiency”).
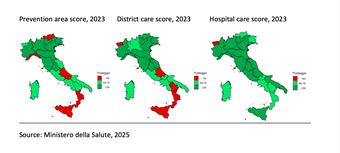
The data published at the end of February 2025 illustrate a mixed picture: while some regions show steady progress, persistent territorial inequalities and structural weaknesses in district care and prevention remain critical. These gaps not only hinder equitable access to healthcare but also increase pressure on hospital facilities, threatening the overall sustainability of the system.
Main results
The analysis of the 24 core indicators (a subsample of the total 88 indicators) reveals contrasting trends between 2019 and 2023. Hospital care shows improvement, while district care and prevention services continue to decline. Failures in these areas are classified as non-compliances, blocking access to incentive funds from the National Health Fund.
In 2023, regions such as Piedmont, Lombardy, the Autonomous Province of Trento, Veneto, Friuli–Venezia Giulia, Emilia-Romagna, Tuscany, Umbria, Marche, Lazio, Campania, Puglia and Sardinia scored above the sufficiency threshold of 60 across all macro-areas (see Figure 1). Notably, no region or autonomous province scored below the threshold in all three areas, yet several struggled in one or more sectors:
Below the threshold in two macro-areas: Valle d’Aosta (District and Hospital), Abruzzo, Calabria, Sicily (prevention and District).
Below the threshold in one macro-area: Autonomous Province of Bolzano, Liguria and Molise (prevention), Basilicata (district).
Figure 1 visually represents regional performance, emphasizing the territorial disparities and highlighting areas requiring urgent intervention. The COVID-19 pandemic underscored the fragility of local healthcare networks, yet this remains an unresolved weakness in many regions. The lack of robust prevention strategies contributes to higher incidences of avoidable diseases, exacerbating hospital overcrowding, inflating costs and worsening long-term health outcomes.
Analysis
Despite the ambitious investment of over EUR 7 billion allocated by the National Recovery and Resilience Plan (NRRP) to strengthen and reorganize primary care – with initiatives ranging from the creation of community health centres and community hospitals to the enhancement of territorial and digital healthcare – significant doubts remain about the feasibility of achieving the objectives by the June 2026 deadline. The challenges related to infrastructure implementation timelines, healthcare staff shortages, and the varying capacities of Regions to carry out reforms could undermine the overall effectiveness of the investment.
Overall, the NHS shows an improving trend in the hospital sector, while the areas of district care and prevention continue to worsen, albeit with a less “robust” trend. Particular attention should be paid to the trend in district/primary care. In fact, in 2023 the first effects of the adoption of the standards referred to in Ministerial Decree 77/2022 were expected, but did not materialize. That decree provided for the implementation of what was envisaged and financed by the NRRP for the revitalization of services, starting with community health centres, community hospitals, and integrated home care. These data, on the other hand, seem to signal a new alarm bell, indicating that the main problem of the NHS remains the fragility of district care that was exposed during the COVID-19 emergency period, especially in some districts, despite the interventions and investments put in place in recent years.
In conclusion, the LEA results provide valuable insights into regional healthcare performance, revealing both progress and persistent vulnerabilities. Strengthening district care and prevention systems is essential to balancing the system, alleviating hospital strain, and enhancing health outcomes. These results point to the need to address structural and organizational barriers, ensuring that the opportunities presented by the NRRP translate into sustainable, long-term improvements in healthcare equity and access.