Nataliia Piven, Jarno Habicht
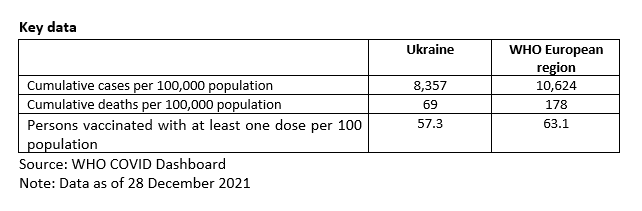
Note: This document reflects the situation in Ukraine on 28 December 2021.
Introduction
This snapshot explores the role of public health agencies and services in Ukraine in responding to the COVID-19 pandemic. It uses a sub-set of public health functions to serve as ‘tracers’ of how far public health was engaged in different aspects of the response to the pandemic. The snapshot covers the role of public health agencies and services in the following areas: pandemic planning, overall governance of the pandemic response, guidance on non-pharmaceutical interventions, communication, testing and tracing, and vaccination. The report draws on a review of published evidence, as well as expert interviews.
Pandemic planning
According to the 2019 Global Health Security Index report1, Ukraine's readiness to fight epidemics prior to the COVID-19 pandemic was rated as ’below average‘ (38 points out of 100). Ukraine ranked 94th among 195 countries, indicating that the health security capacities and capabilities needed to prevent, detect, and respond to significant infectious disease outbreaks were suboptimal. This is also a consequence of the prolonged transformation and development of the health system in Ukraine, which has been in the process of making substantive changes to its public health infrastructure since 2015. The transition follows policy recommendations and obligations formulated under the EU-Ukraine Association Agreement of 20142, recommendations on strengthening the national health emergency preparedness and response system issued by the external Global Health Security Agenda Assessment of Ukraine (2015)3 and the 2015 European Centre for Disease Prevention and Control’s (ECDC) assessment of public health governance, surveillance, preparedness and response capacities for communicable diseases.
Between 2017 and 2020, ideas for a new public health system were developed in accordance with the Sustainable Development Strategy Ukraine 20204 and the EU-Ukraine Association Agreement,2 together with its attendant policy recommendations and obligations around communicable disease control5. Prior to the reform, the State Sanitary Service of Ukraine (SES) was responsible for public health in Ukraine. The SES had a centralized structure and financing, and its capacity and activities focused on communicable disease prevention and control through regulation of risk factors and health inspections. The SES did not adequately respond to new public health challenges or comply with modern approaches to disease surveillance, including for noncommunicable diseases (NCDs) and health promotion.
During the first stage of the reform in 2015, the Cabinet of Ministers established the Ukrainian Public Health Centre (UPHC) as an autonomous public institution6. The UPHC would take over the executive functions of the SES as the leading expert institution on public health while remaining subordinate to the Ministry of Health. As a result of the reform, the epidemiological surveillance function of the SES was transferred to the Ministry of Health, whereas inspectorate functions related to business operations’ compliance with sanitary legislation were transferred to the State Service on Food Safety and Consumer Protection.
The UPHC was established with a modern, broader public health mandate. The mission of the UPHC is to ensure quality of life and health of the Ukrainian population through disease prevention, health promotion and protection, counteracting potential health threats, ensuring an effective response to public health emergencies, and engaging in information and communication. Its mandate includes public health monitoring of diseases, epidemiological surveillance and biosafety, group and population prevention of diseases, response to epidemics and strategic governance in public health.
The Ministry of Health and the UPHC are the main public health entities directly engaged in the overall response to the COVID-19 pandemic at the national level through the activation of the national emergency response mechanism under a single state civil protection system, as outlined in the Civil Protection Code of Ukraine. They are supported by the state Budget Programme ‘On Public Health and measures to combat epidemics’, which assigns responsibility for the planning of activities to prevent public health emergencies.
At a sub-national level, public health infrastructure is represented by two types of agencies with different levels of subordination, governance arrangements, budgeting, accountability, as well as operational and technical capacities. This organizational duality in public health service delivery was an outcome of the uncompleted second stage of the public health reform as set out in the Concept for the Development of the Public Health System (2016)7 and the Action Plan for Implementation (2017)8. These documents laid the foundation for the future development of the public health system with a vision for health promotion, disease prevention and health protection aimed at increasing life expectancy and quality of life and prolonging the active working age through the concerted efforts of society.
The Concept for the Development of the Public Health System7 and decentralization reforms9 envisaged the transfer of certain public health service functions and resources to regional Public Health Centres (rPHCs) under oblast authority to coordinate public health policy implementation at the regional level. The development of rPHCs began in 2017. By 2020 they had been established in all but two oblasts and entrusted with implementation of essential public health operations at the regional level10. At the same time, the network of Oblast Laboratory Centres of the Ministry of Health (OLCs), which was inherited from the abolished SES and is mandated to maintain implementation of certain public health services, continued to function in full through verticalized central governance. These services are related to routine and event-based epidemiological surveillance, emergency preparedness, immunoprophylaxis and data collection, as outlined in the State Budget Programme ’Public health and measures to combat epidemics‘.
The first case of COVID-19 in Ukraine was detected on 29 February 2020. Before the COVID-19 outbreak was declared, two parallel public health systems were in place at regional level. However, a clearly delineated distribution of public health functions among both types of public health institutions (rPHCs and OLCs) and across different levels of government was lacking. This situation exposed potential fragmentation in the delivery and funding of public health services, with regard to health emergency governance and planning. One year later, COVID-19 has refocused the Government of Ukraine’s vision for the architecture of the public health system11 and led to several decisions on its reconfiguration towards more verticalized governance12.
This entails the reorganization of PHCs (regional, Kyiv) through their merger with health care facilities of the respective administrative-territorial units and transfer of their staff to OLCs, transforming these into Oblast Centres for Disease Prevention and Control (OCDCs) which are authorized to be single public health institutions at the regional level from 1 July 2021.
Ukraine did not have a specific national pandemic response plan (e.g. influenza preparedness plan) in place before the outbreak started. Within the context of the ongoing transformation of the public health system and the legislative gap in assigning national, regional and local responsibilities on planning and response to public health emergencies, there was a lack of clarity around the specific role of public health agencies, as mentioned above. This created an extra challenge for the Ministry of Health and the Ukrainian Public Health Centre’s coordination of the COVID-19 pandemic response.
With the activation of the Operational Emergency Committee in February 2020, the Government reinstated the position of the Chief State Sanitary Doctor of Ukraine to ensure proper coordination of the COVID-19 response by the Ministry of Health. Following the execution of the framework of civil protection, the Chief State Sanitary Doctor of Ukraine was assigned as Head of activities with regard to COVID-19. The National COVID-19 Emergency Response Headquarter (‘Shtab’, hereafter referred to as Ministry of Health COVID-19 Headquarter), which functions as a multisectoral executive structure with representation from different sectors engaged in the response to COVID-19, was established. It is tasked with regular situation analysis, identification of operational needs, planning of workforce and resources, organization and coordination of the intersectoral response, communication with the public etc. Most members of the Ministry of Health COVID-19 Headquarter are representatives of the UPHC. This is mainly attributable to the key role of the UPHC as the national public health agency responsible for epidemiological surveillance, data analysis, organization of laboratory testing, and management of the stock of medicines at national and regional levels, as well as being the authorized national coordinator for the International Health Regulations (IHR).
The UPHC’s engagement in planning the response to COVID-19 includes a daily epidemiological situation analysis, the monitoring of hospital bed occupancy, as well as laboratory and testing capacity, and the overall implementation of the COVID-19 vaccination campaign. These activities are synchronized with the regional level of response, led by OCDCs. At the same time the Ministry of Health, together with regional and local authorities, remained responsible for identification of hospitals designated for COVID-19, a responsibility shared with the National Health Service of Ukraine (NHSU) as the single agency for purchasing health services at the national level. Planning for personal protective equipment (PPE) for healthcare workers is primarily the responsibility of healthcare facility owners/managers.
In addition, overall responsibility for the COVID-19 response is being taken by the Government and the Prime Minister as Head of the National Emergency Council. Expert public health advice to the Government for decision-making purposes is provided by the Chief State Sanitary Doctor, but there is no convincing mechanism to monitor whether the advice given follows the evidence generated by the UPHC and whether this evidence supports the decisions being made.
The active and broad engagement by the newly established national public health institution (the UPHC)6 highlighted its role as a leading expert institution in the area of public health. This has also been reflected in newly drafted legislation on the public health system13. However, the overall role of the UPHC in planning for public health emergencies remains uncertain due to the complicated nature of the emergency response via civil protection mechanisms, where the role of public health institutions such as the UPHC and OCDCs is neither specified in, nor supported by, a legislative framework.
The preliminary lessons of the COVID-19 pandemic have highlighted system bottlenecks and triggered special attention to the public health system by the Government and politicians. The pandemic crisis has become a challenge, as well as a window of opportunity, for public health institutions at national and regional levels to upgrade their technical, functional and infrastructural capacity through improved laboratory equipment, implementation of electronic tools for surveillance and tracing of contacts etc. However, more needs to be done at policy and operational levels to ensure better planning for emergency preparedness in the future.
Overall governance of the pandemic response – including the role of public health agencies in providing scientific guidance
The national emergency response system is a single state civil protection system based on the Civil Protection Code of Ukraine. A clear vertical response system is governed by Emergency Councils (i.e. the National and Regional Commissions on Technogenic and Ecological Safety and Emergency Situations, led by the Prime Minister and regional Governors in each oblast, respectively) and Emergency Task Forces (i.e. Commissions on elimination of the consequences of the national-level and regional-level medical and biological emergencies of natural origin associated with the spread of COVID-19) as well as the Emergency Response Headquarters - “shtaby” – which are the main executive bodies.
Starting from 3 February 2020, the Cabinet of Ministers activated the Operational Emergency Committee, headed by the Prime Minister. Similar mechanisms were also triggered in each region. At the same time, the Cabinet reinstated the position of the Chief State Sanitary Doctor of Ukraine and assigned it to one of the Deputy Ministers of Health, who was tasked with coordinating the Ministry of Health’s response to COVID-19, leading the Ministry of Health COVID-19 Headquarter and coordinating emergency response activities in an “emergency situation mode”. Thus, governance in response to COVID-19 pandemic was de facto delegated to the Chief State Sanitary Doctor of Ukraine, who is able to mobilize civil protection resources from other state authorities, including regional authorities. However, several decisions which currently do not fall within the responsibility of the Ministry of Health should in fact be directed by the Ministry of Health, in line with the Chief State Sanitary Doctor’s advice/proposals to the Government.
At the same time, the Presidential Office and the National Security Council continue to monitor and retain overall control over the COVID-19 situation through the Main Situation Centre of Ukraine14 as well as regular meetings with a wide range of national and regional authorities, professional and business entities and civil societies. Several resolutions addressed to the Government, with a list of actions to be followed so that the public health and socio-economic situation arising as a consequence of the pandemic can be improved, have been issued by the President.
The Ministry of Health, the Chief State Sanitary Doctor and the UPHC are permanent members of the meetings, but there is no publicly available evidence on how far scientific advice was considered during the decision-making process. The role of UPHC within the national governance response mechanism is not officially documented, but the representation of UPHC staff within the Ministry of Health COVID-19 Headquarter allows this key national public health institution to provide its expertise, with a limited capacity to influence decision-making or the direct coordination of the response.
The regional Public Health Response Monitor15 which was launched in Ukraine in March 2020 highlighted the limited governance of regional level public health institutions (OLCs) as a result of an overall insufficient legislative framework. Although general principles for the operation of the emergency executive bodies (‘shtabs’) are outlined in the Civil Protection Code, their roles and responsibilities at regional level are neither officially documented nor clearly identified. This was reflected across regions by a wide variety of overall governance modalities and of levels of engagement by public health institutions in response to the pandemic. For example, coordination of epidemiological surveillance, communication, reporting to the national level, laboratory testing and stocks management are carried out by two key regional bodies: the Oblast Health Departments of the Regional State Administration and the Laboratory Centers of the Ministry of Health (transformed into OCDCs in 2021).
Nonetheless, membership of regional public health institutions in regional ‘shtabs’ (including some cases where heads of OLCs (OCDCs) were appointed as ‘shtab’ Heads or Deputy Heads) has improved both intersectoral cooperation and coordination between regional stakeholders as well as vertical coordination between national and regional ‘shtabs’. Compared to the pre-pandemic period, this was a positive development because the abolishment of the SES in 2015 had led to uncertainty around the role of OLCs during public health emergencies.
In the meantime, considering that Ukraine remains in the process of reforming its public health system, lessons can be drawn about the designation and operationalization of the new public health model and about clearly delineating the role of key public health institutions in specific public health legislation (which is pending in Parliament) and subsequent by-laws.
Guidance on non-pharmaceutical interventions – in particular the use of masks, social distancing and lockdown
After the first COVID-19 case in Ukraine was confirmed on 3 March 2020, quarantine16 and restrictive measures were introduced by the Government on 12 March 2020 and initially remained in effect until 3 April 2020. The government declared an emergency situation on 25 March 2020. The measures were subsequently extended several times in adjusted modalities following a ‘zoning strategy’. They remained in force as of September 2021.
In accordance with the law ‘On protection of the population from infectious diseases’16, the decision to introduce quarantine was made by the Cabinet of Ministers, based on the request by the Ministry of Health at the behest of the Chief State Sanitary Doctor. The announcement by the Cabinet of Ministers specifies the circumstances that led to the introduction of quarantine and introduces non-pharmaceutical individual and societal interventions. Among others, these outline the boundaries of the territory under quarantine; approve the necessary preventive, anti-epidemic measures; delineate implementing agencies and deadlines; set temporary restrictions on the rights of individuals and legal entities and outline additional responsibilities; and set out the grounds and procedures for mandatory self-isolation, and a person’s stay under observation or hospitalization in temporary health care facilities (e.g. specialized hospitals).
In practice, the legislation offers clear guidance for the introduction of public health and social measures and describes the leading role of the Ministry of Health and the Chief State Sanitary Doctor. However, it does not outline the role of UPHC as the main expert public health institution, and its influence on decision-making is limited to giving advice at the level of the Ministry of Health Emergency Headquarter (‘shtab’). Given this legislative context, the Ministry of Health facilitates the introduction of strict public health and social measures for approval by the Cabinet of Ministers, while overall guidance and communication with the public remains under the responsibility of the Ministry of Health, supported by UPHC expertise.
From the beginning of pandemic, giving due consideration to the epidemiological situation, the Ministry of Health made several proposals regarding the introduction or/and easing of restrictive measures. These are being adjusted in line with the evolving epidemiological situation and thus far have included the following measures: strategies on wearing face masks or respirators that cover the nose and mouth and maintaining a physical distance of at least 1-1.5 metres; specific requirements for self-isolation, border crossings, organization of mass-gathering events, closure of schools and the operation of different types of business; passenger transportation and domestic movements etc.
More detailed guidance was supported by recommendations issued regularly by the Chief Sanitary Doctor17 on the organization of anti-epidemic measures for services or businesses such as beauty salons; restaurants; trade in food and non-food goods; work in office spaces; dental services; long-term facilities (including mental health, social care homes); hotels; road passenger transportation; educational processes; kindergartens; metro; gyms and pools; football matches among professional football clubs; railway passenger transportation; trade in market places (rynok/bazar); organization of cultural and artistic events; organization of anti-epidemic measures in some enterprises, institutions and organizations for the youth and the sphere of national-patriotic education; etc.
While the introduction of appropriate public health and social measures is an important strategy, enforcement of these measures is equally important. The monitoring of the population’s and businesses’ compliance with restrictive measures does not fall within the remit of public health agencies. Enforcement is carried out by the olice, the State Labor Service inspectors and the Food Safety and Consumer Protection Service, which have the capacity to impose fines.
In order to conduct a deeper analysis of the public health and social measures (PHSM), the WHO Country Office for Ukraine conducted two rounds of PHSM enforcement monitoring across all the regions of Ukraine during the first lockdown in January 2021 and during the Orthodox Easter weekends in May 2021. The results demonstrated that most establishments followed the rules or restrictions imposed by the Government. At the same time, violations were recorded with regards to proper wearing of masks, keeping an appropriate physical distance in queues, and compliance with restrictions in public transport and religious places. The communication strategies and plans of public health agencies at national and regional level would benefit from awareness campaigns about precautionary measures and behaviours.
Communications strategy and communicating with the public
The overall communications strategy was led by the Ministry of Health. Starting with daily media briefings made by the Chief State Sanitary Doctor or the Minister of Health, it subsequently extended to dissemination of information through official dashboards, social media and messenger chart-bots. Between January and March 2020, WHO recommendations on hand hygiene and respiratory etiquette were translated into the Ukrainian language and posted in different formats on social media channels, such the social media pages of UPHC18, the Ministry of Health19, and the WHO Country Office in Ukraine20 as well as on their official web pages.
Additionally, in early March 2020, the Cabinet of Ministers set up a website (https://covid19.com.ua/) containing recommendations on hand hygiene and respiratory etiquette, while at the same time Ministry of Health launched a Coronavirus channel21 on the messaging platform ‘Telegram’. Furthermore, the National Health Service of Ukraine (NHSU) regularly provides updates to patients and healthcare workers, as well as to local governments.
Shortly before the movement restrictions which took effect on 12 March 2020, recommendations on social distancing were issued and posted through official Ministry of Health and UPHC channels. In November 2020, the All-Ukrainian Contact Centre of the Ministry of Health for Combating Coronavirus Disease began its work on a 24/7 basis with 150 operators involved.
The Directorate of regional development and decentralization of the Presidential Office of Ukraine also communicated with the general population via a monitoring dashboard22 which published information on hospitalized suspected and confirmed cases. In April 2020, the National Health Service of Ukraine launched a chat bot23 with COVID-19 instructions for physicians, ambulances, local authorities and patients, while the UPHC launched a website24 that gathers up-to-date information on coronavirus infections for healthcare professionals. Furthermore, in order to increase access to up-to-date information on responding to the pandemic for national and regional health workers, the UPHC, the Ministry of Health and the WHO Country Office in Ukraine jointly launched a new distance learning platform in September 2021. This contains comprehensive courses for specialists engaged in disease prevention, investigation, detection and pandemic response. Several WHO courses are available on the platform, including courses on epidemiological surveillance; COVID-19 epidemiology, outbreak prevention and control; “Application of ELISA for COVID-19 Data Management” and “Go.Data - field data collection, disease transmission chains and contact tracing software”.
Together with the UPHC, the WHO Country Office in Ukraine has conducted more than 10 rounds of the Behaviour Insights Study which aims to provide support to Ukrainian authorities in formative research about citizens’ risk perceptions, knowledge and behaviour linked to COVID-19, which can be used to adjust population messaging.
The roll-out of the COVID-19 vaccination campaign was also supported through the launch of the COVID-19 vaccination information portal25, where all relevant and reliable information on the course of the vaccination campaign in Ukraine is published. A Communication Centre was also established at the UPHC to provide information on the vaccination campaign, to promote vaccination and provide evidence-based information about COVID-19 vaccines.
In order to ensure that information reaches speakers of other languages, the Ministry of Health, together with the Ministry of Culture, translated COVID-19-related information material, including infographics, into 13 minority languages,
The Ministry of Health and the UPHC have no joint communication strategy. Despite having significantly contributed to government communications as a main source of daily information on the epidemiological situation, the UPHC did not have a primary role of communicating with the public.
The regional Public Health Response Monitor identified the following features of regional communication strategies:
- Health communication varies across regions and is coordinated by different authorities such as the Communication Department and Health Department; by OLCs (OCDCs); regional Public Health Centres or Heads of Emergency Task Forces or by the Governor's press service;
- Official spokespersons for the COVID-19 outbreak and the most authoritative specialists have been appointed to speak to the mass media in many regions, mostly represented by the Governor or the Regional Chief Sanitary Doctor;
- In some regions, the Red Cross has been actively engaged in communication activities;
- Ministry of Health guidelines and WHO guidance and recommendations that have been translated into Ukrainian are mainly transmitted from the national to the regional and local levels through Health Departments and OLCs (OCDCs);
- The majority of regions created a special webpage within Regional State Administration websites to provide the population with information related to COVID-19 with links to national sources;
- Task forces to monitor the media and social networks have been created in some regions in order to identify and respond to fake news, reduce social tension and prevent panic among residents of the region;
- Social networks are actively used in all regions to communicate up-to-date information on the epidemiological situation and COVID-19 prevention measures (hygiene and respiratory etiquette, physical distancing etc.);
- COVID-19 hotlines for both the population and health workers have been set up in all regions.
A conclusion that can be drawn so far is that the role of public health institutions in crisis communication needs to be strengthened in the future, taking into account behavioural insights.
Testing and tracing
Throughout the pandemic, the UPHC and the network of OLCs (OCDCs) were and continue to be responsible for testing and tracing. National testing and tracing strategies are established by the Ministry of Health following the expertise and recommendations from UPHC. According to the national guideline for COVID-19 management, family doctors or healthcare facilities (primary health care facilities or hospitals) should refer all suspected cases that meet the national case definition to OLCs (OCDCs) in the respective territories. Testing is largely conducted by the OLCs (OCDCs), with samples being tested by private laboratories, laboratories in hospitals, HIV laboratories and laboratories in the veterinary sector. The laboratories outside the public health system (including private laboratories) are responsible for reporting positive PCR-test results to the doctor of the referred patient. Furthermore, the OLC (OCDC) is notified. Data are then consolidated and integrated into surveillance reporting systems on a daily basis.
By the end of September 2021, the share of tests done in the private sector was around 28%. No new laboratory structures have been set up to extend testing capacity, but several OLC (OCDC) facilities have been renovated. All OLCs (OCDCs) were equipped with one to three thermo cyclers and 25 new RT-PCR thermocyclers have been procured. Furthermore, new semi-automatic extraction equipment was installed at the UPHC and almost all OLCs (OCDCs).
Ukraine has limited capacity to sequence many samples from SARS-COV-2 confirmed cases and support is being provided by international reference laboratories. During pre-screening to select appropriate samples for sequencing, UPHC conducts SNP-typing to detect N501Y mutation characteristics for variants of concern. Although the national sequencing strategy foresees four sequencing labs: the UPHC in Kyiv, the Anti-Plague Institute in Odesa and the Kharkiv and Lviv Oblast Laboratory Centers. The UPHC launched the whole genome sequencing during September – October 2021.
The UPHC shared a leading role in the designation of the national testing strategy, considering the epidemiological situation and laboratory capacity across the country. A COVID-19 National Reference Laboratory, based at the Virology Laboratory of the UPHC, has been established. The UPHC also serves as a mentoring centre for all 25 OLCs (OCDCs).
The UPHC and the OLCs (OCDCs) were constantly provided with technical expertise, support and advice with regards to strengthening testing and tracing capacities (e.g. strategy adjustment, planning of resources, delivery of testing materials and new laboratory equipment, capacity-building interventions for laboratory staff and epidemiologists, application of digital tools etc.) by the WHO Country Office in Ukraine.
Several online workshops on laboratory biosafety and biosecurity were conducted by WHO and the UPHC, particularly on “Biosafety cabinets operation”, “Personal protective equipment”, “Disinfection and decontamination”, “Good microbiological practices”, “Methods of detection and identification of SARS-CoV-2 variants of concern”. Several on-site training sessions on laboratory biosafety and real-time PCR were also provided.
At the beginning of the epidemic in Ukraine, testing capacity was very low, increasing from 200 tests per day initially to 49,323 in November 2020 and around 57,000 in April 2021. The Government and the Ministry of Health in particular were criticised for very low testing coverage. In May 2020, the Ministry of Health introduced amendments to the national COVID-19 guidance (Ministry of Health Order #722 of 28 March 2020) and supplemented the testing strategy with ELISA testing. Starting from December 2020, the testing strategy was supplemented by the use of Antigen Rapid Diagnostic Test (Ag-RDT) to expand testing coverage and identification of cases. The Ag-RDT is performed by primary healthcare doctors, hospitals and state and private laboratories to confirm suspected SARS-CoV-2 cases with symptoms. The national algorithm requires a symptomatic suspected case with negative Ag-RDT to conduct PCR test, whereas those with a positive Ag-RDT result are immediately classified as confirmed cases. The change has made testing more accessible at district level through to the primary healthcare level and eased the workload on OLCs (OCDCs).
Since all suspected cases are reported to the OLCs (OCDCs) in the respective territory, epidemiologists at the OLCs (OCDCs) conduct epidemiological investigations which also include close contact tracing of persons who are/were:
(i) residing in a household with a COVID-19 case
(ii) in direct physical contact with a COVID-19 case
(iii) in direct contact with respiratory discharge (sputum) of a COVID-19 patient
(iv) have been within 2 meters’ distance of a COVID-19 patient for at least 15 minutes
(v) health workers or other persons taking care of a COVID-19 patient or lab personnel handling samples from COVID-19 patients without proper (or misusing) personal protective equipment
(vi) have been seated within two seats in any direction of the COVID-19 case during travel by airplane, or other co-travellers and crew members if there is reason to believe that there is a wider risk of exposure.
Contact tracing and monitoring is generally organized by OLC (OCDC) epidemiologists with involvement of primary healthcare workers through remote mode (phone, online communications) or personal visits. Contact tracing is also supported by the digital mobile application ‘Diya’ (‘Act at home’)27 to monitor citizens undergoing 14-days of self-isolation using GPS data, but this has not yet been applied to trace contacts.
Since 22 May 2020, 14 days of self-isolation are mandatory if:
(i) a person had contact with a patient with COVID-19;
(ii) a person crossed the state border or crossed the checkpoints of entry into and exit from the temporarily occupied territory of Ukraine.
Supervision of a person's stay in a place of self-isolation is carried out by:
(i) employees of the National Police, the National Guard (following the internal order of measures to control self-isolation), state institutions of the epidemiological profile of the Ministry of Health, and authorized local government officials; or
(ii) through using the mobile application ‘Diya’. Installation of the ‘Diya’ application is voluntary.
The situation around tracing of contacts is challenging. A national strategy to guide contact tracing approaches at regional and local levels with clear performance indicators and to collect information on contacts to enable formulation of evidence-based policy recommendations is lacking. Existing contact tracing procedures and practices are region-specific and vary significantly across regions due to different capacities and limited availability of people who can be trained to conduct effective contact tracing.
To help implement a contact tracing programme for COVID-19 in Ukraine, the WHO Country Office has been providing support, equipment and staff training to Chernivtsi and Odessa OCDC in a pilot project that could be rolled out to other areas of the country. Training was provided to 99 employees of Chernivtsi OCDC and 102 employees of Odessa OCDC on the basics of contact tracing, use of the Go.Data software (an app developed by the WHO’s Global Outbreak Alert and Response Network (GOARN) used in over 35 countries to manage epidemiological data and facilitate faster and more accurate outbreak investigations during public health emergencies) and ways to collect and analyse data. Additionally, the online course “Introduction to Go.Data – Field data collection, chains of transmission and contact follow-up” is available on the Open WHO education platform and UPHC educational portal28. The training is expected to provide healthcare specialists with up-to-date theoretical and practical knowledge on Go.Data software for contact tracing of COVID-19 cases.
There is substantial interest in scaling up this approach to other regions of Ukraine to ensure a high level of epidemiological surveillance and case investigation to improve rapid responses to COVID-19.
Vaccination efforts
The Ministry of Health, the Chief State Sanitary Doctor of Ukraine, UPHC, the National Technical Advisory Group’s (NITAG) and the Ministry of Health Task Force on Vaccine-Preventable Diseases (hereafter – Ministry of Health VPDs Task Force) all play a strategic role in the planning and coordination of the mass vaccination campaign. Health departments of oblast administrations and the regional coordinators for the vaccination campaign are key implementing partners and coordinators at sub-national level, guided operationally by the Chief State Sanitary Doctor and the national vaccination coordinator from the UPHC. Regional vaccination coordinators are mostly from Health Departments and, in some regions, from the OCDCs. This indicates a suboptimal level of engagement of regional public health institutions (OCDCs) in the vaccination campaign, which potentially needs to be improved by strengthening the capacity of immunization units within OCDCs.
The preparatory work for the COVID-19 vaccination campaign began in September 2020. Following a resolution by the Chief State Sanitary Doctor of Ukraine, a working group of national experts and representatives of international partners (including WHO, the World Bank, UNICEF, and the United States Centers for Disease Control and Prevention) with involvement of national experts from the National Technical Advisory Group (NITAG)29 developed practical recommendations for the COVID-19 coronavirus vaccination campaign in Ukraine and provided criteria for prioritizing groups for immunization.
The Ministry of Health VPD Task Force, the main multi-stakeholder platform including international partners aimed at coordinating the COVID-19 vaccination campaign at the national strategic level, was established in 2019, before the pandemic. It was activated in 2020 to facilitate the COVID-19 vaccination campaign and serves as a decision-making body where each decision made is enforced by a Ministry of Health Order. Several important strategic decisions have been taken by the Ministry of Health VPDs Task Force, namely on the communication strategy and its implementation, procurement and logistics, staff training, creation of vaccination lists and records, management of vaccination data, pharmacovigilance, etc.
Following NITAG recommendations, the Ministry of Health VPDs Task Force approved nine priority groups for COVID-19 vaccination. These include (in order of priority access to vaccination):
- health professionals, particularly frontline responders to the pandemic;
- social workers;
- persons living in long-term care facilities and employees of such institutions; - older people (60 years of age and older), including those with comorbidities who are at risk of complications and death due to COVID-19; with the sub-priority in this group starting with people aged 85 years (highest priority), and then divided into cohorts 80-84 years, 75-79 years, 70-74 years, 65-69 years and 60-64 years;
- servicemen participating in the Joint Forces Operation;
- employees of critical state security structures, including the State Emergency Service, the National Police, the National Guard, the Security Service, the State Border Guard Service e, servicemen of the Armed Forces of Ukraine, the Ministry of Internal Affairs of Ukraine;
- teachers and other workers in the field of education;
- adults (18 to 59 years of age) with comorbidities who are at risk for complications and death due to COVID-19;
- people in detention facilities.
NITAG conducted several meetings on the COVID-19 vaccination response and provided the Ministry of Health with technical recommendations30 regarding the prioritization of particular groups for COVID-19 vaccination; COVID-19 vaccination for people aged over 65 years, those recovered after COVID-19, people with cancer, vaccination of contacts with confirmed cases etc. All the recommendations were taken into consideration by the Ministry of Health and reflected in consequent decisions, particularly in the approved Roadmap for the introduction of COVID-19 vaccines and the implementation of mass vaccination (hereafter – the Roadmap).
Through endorsement of the Roadmap, Ukraine launched a multi-level (five-stage) COVID-19 vaccination campaign to cover at least 50% of the country's population during 2021 and 2022. Data on the number of priority groups for vaccination were provided by the UPHC considering the information from regions, central executive bodies, the State Statistics Service of Ukraine and the Centre for Medical Statistics of the Ministry of Health. From 21 July 2021, Ukraine launched the fifth stage of the vaccination campaign for all adults aged 18 years and older who are not in priority groups. Based on the Roadmap and following approved national plans, regional (oblast) vaccination plans were developed and activated under operational coordination by the regional coordinators and supervision at the national level. The vaccination campaign is being implemented at facility-level vaccination points for people over 60 and those aged 18-59 with concomitant diseases; through deployment of mobile vaccination teams for professional groups (health workers, teachers etc.), organizations with more than 50 people in the team, low-mobility groups; and mass-vaccination centres deployed in public administration facilities, stadiums, shopping malls, airports etc for all others aged over 18 years. To ensure sufficient coverage, COVID-19 vaccination was introduced by the National Health Service of Ukraine in the Programme of Medical Guarantees in 2021.
Additionally, the vaccination campaign was supported by the Cabinet of Ministers Resolution of 12 April 2021 which approved the National COVID-19 Vaccination Plan up to 31 December 2021. The plan provides indications for a minimum of vaccination shots by vaccines procured through the central budget or received through the COVAX initiative.
The system of supply, delivery and storage of vaccines in Ukraine has four levels:
- National level – a single storage and supply point is provided by the Ministry of Health State Enterprise ‘Ukrvaktsina’ with the ability to store vaccines for 6 months at temperatures of -20°C and from + 2°C to + 8°C. Vaccines are distributed by ‘Ukrvaktsina’ over a one-month period to up to 25 sub-national (regional) warehouses. The distribution list for the entire batch of vaccines is set by the Ministry of Health.
- Regional (oblast) level – there are 25 storage points at the regional level. The stock of vaccines received from the national level is immediately distributed to the district level, or stored and periodically distributed among the districts at least once a month.
- District level – There are 490 storage points at district level. Health care facilities (mostly primary health care facilities where vaccination points are located) independently collect vaccines from the regional level storage points and deliver them to vaccination points as needed, or at least once a month.
- Permanent vaccination points – There are 11,346 permanent vaccination points. In order to vaccinate against COVID-19 in a way that does not interrupt routine immunization, the Ministry of Health deployed 4,250 additional vaccination points specifically for COVID-19 vaccination, which required provision of additional appropriate refrigeration and ancillary equipment to ensure maintenance of the cold chain.
The role of the UPHC in supporting and coordinating services for vaccine supply and delivery involved calculating distribution needs, verifying the regional population determined for vaccination and determining the possibility of using vaccines before their expiry date. The UPHC also conducted analyses of existing refrigeration equipment used for storage of medicines and vaccines at different levels of the cold chain and identified further procurement needs. At the same time, appropriate management of the supply system was mainly supported by international partners.
Overall, the COVID-19 vaccination campaign represents a substantial challenge for the public health system and the UPHC in particular. System performance bottlenecks which appeared during the measles outbreak of 2017-2019 became prominent again during the COVID-19 crisis. There is an acute need for a series of systemic transformations to ensure undisrupted and well-coordinated implementation of immunization programmes in the future. Despite a high level of commitment by the Government and the Ministry of Health and the UPHC’s efforts to improve routine vaccination coverage in recent years, levels of vaccine hesitancy among the population in Ukraine are too high and remain a challenge for the COVID-19 vaccination campaign.
On 26 November 2020, Ukraine’s Vaccine Request to the GAVI COVAX Facility was discussed and approved by the Ministry of Health VPDs Task Force. Irrespective of the chosen vaccination scheme, Ukraine expected to receive vaccine doses in quantities equal to 20% of its population size, approximately 8,346,555 doses by the end of 2021. As of 24 September 2021, Ukraine received 4,325,910 doses of different vaccines (Pfizer, Moderna and AstraZeneca) delivered by UNICEF through the COVAX initiative. Public procurement plans through the central budget for the needs of the vaccination campaign estimated that 13,913,316 doses were required for 2021.
Conclusion
Ukraine has a network of public health institutions that are fully involved in the response to the pandemic. In the conditions of rather limited resources (financial, infrastructural, human resources), public health agencies aim to maintain essential public health interventions at national and regional levels. As a result of the incomplete transformation of the public health system and the absence of a legal framework, the system faces challenges that require attention. A clear delineation of roles and responsibilities between the Ministry of Health and the UPHC and distinguishing policy-making and executive functions among those institutions could contribute to better governance in coordination and operationalization of public health functions, in particular related to preparedness and response to public health emergencies. The secured role of UPHC as the highest professional, politically independent, and technically capable agency in Ukraine (including the capacity to coordinate the network of OCDC) is envisaged as a critical one to ensure evidence-informed public health decision making and accountability for the entire continuum of public health system governance, including needs assessment, planning, and priority-setting.
References
- Nuclear Threat Initiative, Johns Hopkins Center for Health Security & Economist Impact. Global Health Security Index 2019 - Building Collective Action and Accountability.
- European Union & Ukraine. Association Agreement between the European Union and its Member States, of the one part, and Ukraine, of the other part. Official Journal of the European Union (2014).
- Nikkari, S. et al. Global Health Security Agenda Assessment of Ukraine, 2-6 November 2015. Nikkari, Simo Sliter, Karen Weekly, Susan Parente, Paolo Bilukha, Oleg Abuhaimed, Khalid Facelli, Pier Giuseppe Esenamanov, Vasily Bieger, Geoff.
- President of Ukraine. Presidential Decree № 5/2015: “On the sustainable development strategy for Ukraine 2020.” (2015).
- European Parliament & Council of Europe. Regulation (EC) № 851/2004 of the European Parliament and of the Council of 21 April 2004: Establishing a European Centre for Disease Prevention and Control. Official Journal of the European Union (2014).
- Cabinet of Ministers of Ukraine. Order № 909-r/2015: Issues of the Ministry of Health. (2015).
- Cabinet of Ministers of Ukraine. Order № 1002-r/2016: On the approval of the Concept of development of public health system. (2016).
- Cabinet of Ministers of Ukraine. Order № 560-r/2017: On approval of the action plan for the implementation of the Concept of Public Health System Development. (2017).
- The Cabinet of Ministers of Ukraine. Resolution № 333-r/2014: On Concept for reform of local self-government and territorial organization of power in Ukraine. (2014).
- Ministry of Health of Ukraine. Resolution № 2012/2018: About the statement of the Exemplary charter and the Exemplary structure of the center of public health (regional, the cities of Kiev and Sevastopol). (Ukrainian Ministry of Health, 2018).
- Cabinet of Ministers of Ukraine. Resolution № 106/2021: On amendments to the resolution of the Cabinet of Ministers of Ukraine № 1121/2019. (2021).
- Cabinet of Ministers of Ukraine. Resolution № 1121/2021: New public health system: from July 1, disease control and prevention centers will appear in all regions of the country. (Ministry of Health of Ukraine, 2021).
- Parliament of Ukraine. Bill № 4142/2020: Draft Law on the Public Health System. (Parliament of Ukraine, 2021).
- Система моніторингу поширення епідемії коронавірусу. https://covid19.rnbo.gov.ua/.
- World Health Organization. WHO analytical tool helps Ukraine monitor how regions respond to COVID-19. https://www.euro.who.int/en/health-topics/Health-systems/pages/news/news/2020/12/who-analytical-tool-helps-ukraine-monitor-how-regions-respond-to-covid-19 (2020).
- Government of Ukraine. Law № 29/2000: On protection of the population from infectious diseases. 228 (2020).
- Chief State Sanitary Doctor of Ukraine. Resolutions and orders of the Chief State Sanitary Doctor of Ukraine: COVID 19. Official documents and recommendations. https://moz.gov.ua/golovnij-derzhavnij-sanitarnij-likar-ukraini (2021).
- UPHC. Ukrainian Public Health Centre | Facebook. Facebook https://www.facebook.com/phc.org.ua/.
- Ministry of Health Ukraine. Ministry of Health of Ukraine | Facebook. Facebook https://www.facebook.com/moz.ukr/.
- WHO Ukraine. World Health Organization Ukraine | Facebook. Facebook https://www.facebook.com/WHOUkraine/.
- Ministry of Health Ukraine. Coronavirus_info - Coronavirus Project in Ukraine | Telegram. Telegram https://t.me/COVID19_Ukraine.
- Directorate of regional development and decentralization of the Presidential Office of Ukraine. Public dashboard - Covid-19. https://public.tableau.com/app/profile/publicviz/viz/monitor_15841091301660/sheet0.
- National Health Service of Ukraine. Chatbot - Chat with instructions for COVID-19. https://nszu.gov.ua/novini/chat-bot-z-instrukciyami-shchodo-covid-19-226?__cf_chl_jschl_tk__=KVbOOr2pTDX3ko9_RJlyuHukycxbwdVP6I8vJokEUnY-1640169463-0-gaNycGzNCH0 (2020).
- UPHC. Information on COVID-19. https://covid19.phc.org.ua/.
- Vaccination against Covid-19. https://vaccination.covid19.gov.ua/.
- ICIP together with the Ministry of Health and the Council of Europe issued recommendations to combat coronavirus in 13 languages. (2020).
- Ministry of Digital Transformation of Ukraine. ‘Act at Home’ app is launched to counteract the spread of COVID-19 in Ukraine | Cabinet of Ministers of Ukraine. Government Portal https://www.kmu.gov.ua/en/news/yak-pracyuye-zastosunok-dij-vdoma (2020).
- UPHC. Online courses. https://portal.phc.org.ua/uk/view_all_courses/.
- UPHC. National Technical Group of Experts on Immunoprophylaxis. https://phc.org.ua/pro-centr/ntgei (2020).
- NITAG. Meetings of the National Technical Groupof Experts on Immunoprophylaxis. https://phc.org.ua/pro-centr/ntgei/zasidannya-ntgei.